2018长城会(GW-ICC):郑杨教授:透析患者的降压目标及药物选择
2018-10-19 国际循环 国际循环
高血压与肾损害密切相关,透析患者的降压目标及药物选择有其特殊性。GW-ICC 2018大会上,吉林大学第一医院郑杨教授结合相关指南及研究证据,就此话题发表精彩报告,现整理成文以飨读者。图:吉林大学第一医院 郑杨教授高血压是透析患者中的常见表现血液透析患者中高血压患病率达50%~60%以上,腹膜透析患者高血压占近30%。血压与透析患者的全因和心血管事件的关系一直存在争议,一种观点认为血压在
高血压与肾损害密切相关,透析患者的降压目标及药物选择有其特殊性。GW-ICC 2018大会上,吉林大学第一医院郑杨教授结合相关指南及研究证据,就此话题发表精彩报告,现整理成文以飨读者。

高血压是透析患者中的常见表现
血液透析患者中高血压患病率达50%~60%以上,腹膜透析患者高血压占近30%。血压与透析患者的全因和心血管事件的关系一直存在争议,一种观点认为血压在一定范围(如收缩压SBP 110~180 mm Hg),透析前或透析后SBP和舒张压(DBP)与全因和心血管死亡率之间无相关性或呈U型关系;另一种观点则认为透析后高SBP和透析前、后低DBP与死亡率相关,并提示高脉压差(PP)是致病因素。
目前,关于血液透析患者最佳血压目标值尚不清楚,2017年欧洲肾脏病学会、欧洲透析移植协会和欧洲高血压协会共同制定专家共识指出,由于透析期血压不能准确反映患者的实际血压情况,很多因素均可引起患者血压波动,需应用更准确的测量方式,了解患者真实血压水平,即在安静环境、坐位、背部及手臂放松、休息5 min和间隔2 min测量2~3次血压平均值。如果采用家庭血压测量法,则诊断标准为血液透析患者需2周内连续6天非透析日早、晚测量血压,平均BP≥135/85 mm Hg;腹膜透析患者需连续7天,早、晚测量血压平均BP≥135/85 mm Hg。
主要发病机制及治疗
透析患者血压升高的机制包括以下几方面:水、钠排泄能力显著降低,血清钠敏感性较高使钠和容量超负荷;钙磷失衡导致动脉硬化增加;交感神经系统激活;肾素-血管紧张素-醛固酮系统激活;内皮功能障碍;睡眠呼吸暂停;使用重组人促红细胞生成素(rhuEPOs)。
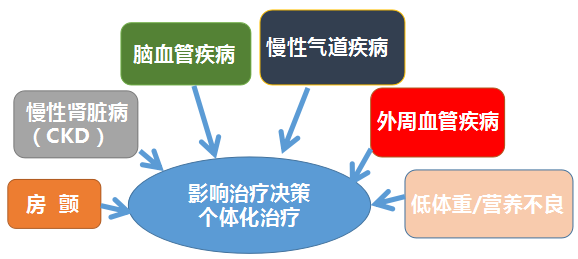
治疗方面,非药物治疗中控制体重很重要,限制钠盐摄入,透析患者钠摄入量≤65 mmol/天(钠:1.5 g,氯化钠:4 g);制定个体化透析液钠浓度;避免使用含钠或钠交换药物;避免透析持续时间过短(<4 h)。药物治疗可选择β受体阻滞剂、血管紧张素转化酶抑制剂(ACEI)和血管紧张素II受体拮抗剂(ARB)、钙通道阻滞剂(CCB)和盐皮质激素受体拮抗剂(MRA)。
此外,利尿剂对终末期肾脏病患者的血压控制无效。在无尿血液透析患者中进行的超声心动图研究表明,静脉注射袢利尿剂,即使大剂量,对中心血流动力学指标的影响也很小。耳毒性高风险,无尿透析患者应避免使用袢利尿剂。肾功能残存(每日尿量>300 ml),血液透析后短时可用袢利尿剂。
药物透析性具有超出血压控制的意义
在血液透析期间去除具有抗心律失常作用的β受体阻滞剂,易发生透析中的心律失常,尤其是在透析引起的血清电解质浓度如钾、钙波动的情况下。血液透析期间不从血浆中去除CCB,因此,不需对这些药物进行透析后补充。ACEI和ARB透析期间药物代谢动力学彼此显著不同,各种β受体阻断剂的透析内动力学也彼此不同。
郑杨教授最后总结中指出,透析患者中常见高血压,尤其是刚开始透析时,而容量扩增是透析患者出现高血压的主要原因,因此,控制容量状态,非常重要。推荐家庭自测血压和动态血压测量方式监测血压,抗高血压药物在透析患者中普遍使用,通常是基于降低血压可降低发病率和提高生存率的信念和达干体重后血压仍持续升高。大多数抗高血压药物可用于透析患者,但应考虑其药代动力学和透析能力,如降压药物应倾向于在傍晚一日1次的给药方案。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#药物选择#
55
#降压目标#
66
#降压#
54
#长城会#
79
#ICC#
62
#GW-ICC#
60
#透析患者#
56