AJOG:TVCL+AFI对PPROM的分娩预测
2015-03-08 Mechront MedSci原创
Mehra S等人进行了一项前瞻性观察研究,以探究经阴道宫颈管长度TVCL和羊水指数AFI,对未足月胎膜早破PPROM孕妇的分娩预测情况。该研究共106名在23-33周孕发生PPROM的宫内单活胎孕妇。其研究成果发表在最新AJOG上。 该研究观察到,106名纳入对象中,有51名(51/106,48%)孕妇在PPROM之后7天内自然分娩。将TVCL进行多因素回归分析得出OR=0.65,95%
Mehra S等人进行了一项前瞻性观察研究,以探究经阴道宫颈管长度TVCL和羊水指数AFI,对未足月胎膜早破PPROM孕妇的分娩预测情况。该研究共106名在23-33周孕发生PPROM的宫内单活胎孕妇。其研究成果发表在最新AJOG上。
该研究观察到,106名纳入对象中,有51名(51/106,48%)孕妇在PPROM之后7天内自然分娩。将TVCL进行多因素回归分析得出OR=0.65,95% CI 0.44-0.97,P<0.05;同理,分析AFI≤5cm得出OR=4.69,95% CI 1.58-13.93,P<0.01。
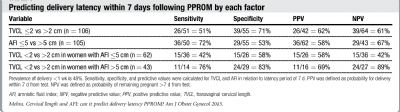
在106名纳入对象中,有42名(40%)孕妇其TVCL≤2cm,62名(59%)孕妇其AFI≤5cm,有26名(25%)孕妇同时满足TVCL≤2cm和AFI≤5cm,有28名(27%)孕妇两者均没有。TVCL≤2cm预测PPROM后7天内分娩的预测值为62%,AFI≤5cm其预测值为58%,TVCL和AFI两者结合其预测值为58%。在两种特征都没有的27名孕妇中,只有3名(11%)孕妇在PPROM之后7天内分娩。TVCL>2cm预测PPROM之后7天内不能分娩的预测值为61%;TVCL>2cm+TVCL≤5cm,其预测值为42%;TVCL>2cm+TVCL>5cm,其预测值为89%。
该研究表明,TVCL≤2cm和AFI≤5cm两个指标可以作为PPROM后7天内分娩的独立预测指标,而TVCL>2cm联合TVCL>5cm则暗示PPROM后7天内分娩的可能性不大。对于临床上PPROM的孕妇,可以根据TVCL和AFI综合母胎情况,评估分娩情况,以及新生儿护理等。
原始出处:
Mehra S, Amon E, Hopkins S, et al. Transvaginal cervical length and amniotic fluid index: can it predict delivery latency following preterm prematurerupture of membranes? Am J Obstet Gynecol 2015;212:400.e1-9.
本文系Medsci原创编译整理!转载需要先获得授权,并附原文链接。谢谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#TVCL#
50
#PROM#
66
#分娩#
51
#PRO#
52