WCLC 2017:再添新桂|王洁教授团队BENEFIT研究证实液体活检指导一线TKI疗效的可行性
2017-10-18 王书航 肿瘤资讯
王洁教授,医学科学院肿瘤医院肿瘤内科,主任医师,教授,博士生导师,国家杰出青年基金获得者,中国抗癌协会肺癌专业委员会常委,北京医学会肿瘤分会副主任委员,中华结核与呼吸杂志、中国肺癌杂志Lung Cancer、Clin. Lung Cancer编委,国家百千万人才工程入选者、获中国突出贡献中青年专家称号,国务院政府特殊津贴获得者。
王书航教授,北京肿瘤医院 胸部肿瘤内科,主治医师,Roswell Park Cancer Institute博士后,梅奥门诊访问学者
2017年WCLC会议第三天的口头汇报,再次传来中国声音。王洁教授团队的 BENEFIT研究为液体活检领域再添新桂。
众所周知,晚期NSCLC已经进入分子分型基础上的个体化治疗新时代。精准的分子分型需要合格的肿瘤组织标本进行检测,然而在临床实践中,部分患者,组织标本不足或难以获得。既往已有很多研究证实血浆ctDNA的EGFR突变检测和组织标本检测结果具有很好的一致性,并已作为一代EGFR TKI的伴随诊断获批。但既往研究均基于回顾性数据,或前瞻性研究的探索性回顾分析。
BENEFIT研究是目前第一项前瞻性的临床研究,进一步明确了ctDNA EGFR突变指导的一线吉非替尼疗效,同时探索EGFR突变等分子标志物的动态变化意义。
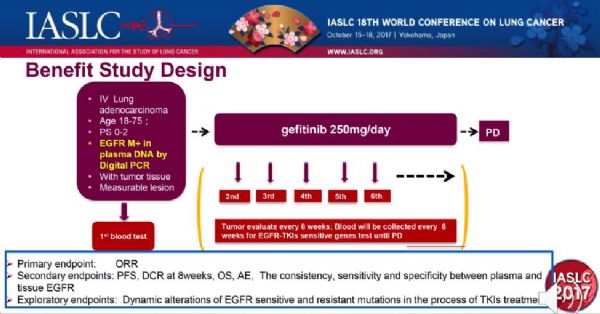
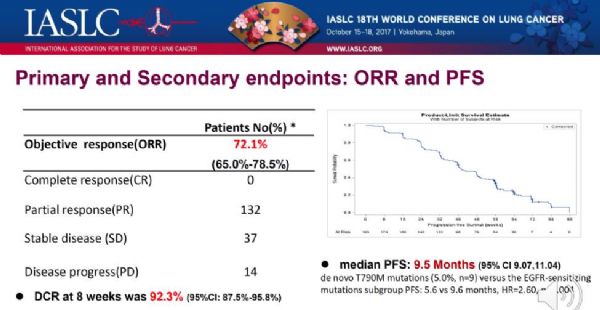
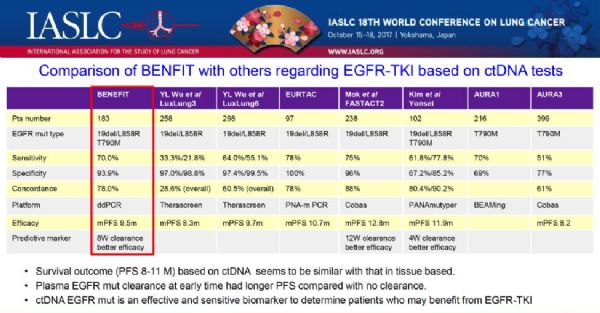
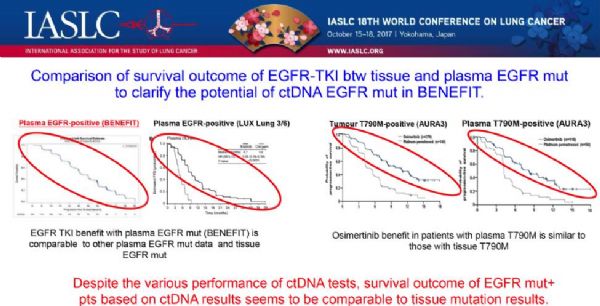
研究的结果显示,ddPCR检测的ctDNA EGFR突变指导的一线吉非替尼治疗的客观有效率为72.1%,治疗8周的疾病控制率为92.3%,中位PFS为9.5个月。该结果与既往IPASS(PFS9.5个月)、 WJTOG 3405 (PFS 9.2个月)等组织EGFR突变基础上的一线EGFR-TKI治疗研究基本一致。
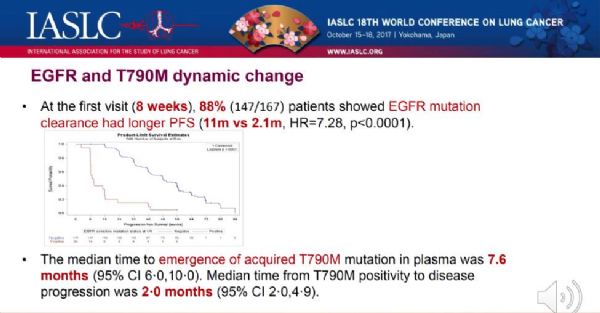
外周血分子标志物的动态监测发现,在治疗的第8周,EGFR突变的检出率与治疗的疗效显着相关,即第8周时EGFR敏感性突变未检出的患者PFS较突变持续阳性的患者显着延长(11m vs 2.1m, HR=7.28, p<0.0001)。该研究同时动态监测了EGFR-TKI耐药基因T790M突变的变化,结果提示T790M突变的中位出现时间为7.6个月(95% CI 6·0,10·0),而从T790M突变出现到疾病进展的中位时间为2个月(95% CI 2·0,4·9),与既往FASTACT2等的研究结果一致,即分子进展可能出现在肿瘤的影像学进展之前,从而提示分子进展或可为三代EGFR-TKI介入的最佳时机,但这一推断仍需临床研究进一步证实,正在进行的 APPLE研究将有助于明确这个问题。
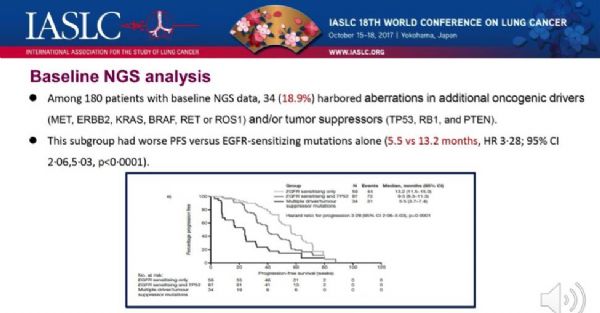
BENEFIT研究同时利用NGS技术分析了基线外周血中多基因的变异。结果提示在180例的患者中,34例(18.9%)携带有除了EGFR突变之外的驱动基因变异(如MET, ERBB2, KRAS, BRAF, RET or ROS1) 和/或抑癌基因的变异(TP53, RB1, and PTEN)。研究将这部分患者分为三组:第1组患者仅携带EGFR敏感性突变,第2组同时具有敏感性EGFR突变和TP53突变,第3组除EGFR敏感性突变还携带其他驱动基因变异(如MET, ERBB2, KRAS, BRAF, RET or ROS1) 和/或抑癌基因的变异(TP53, RB1, and PTEN)。结果提示仅携带EGFR敏感性突变的患者疗效最佳,各组相应的PFS分别为13·0 个月,、9·2 个月以及5.4 个月(HR 3·28; 95% CI 2·06–5·03, p<0·0001)。
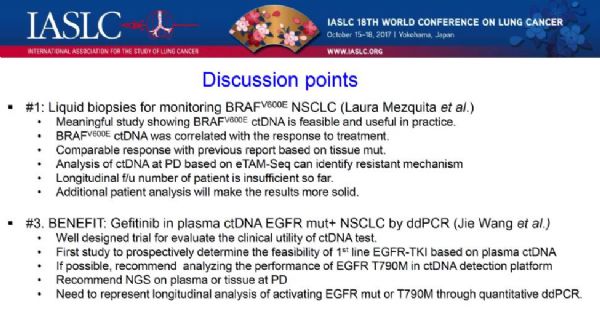
Hye Ryun Kim教授对该研究进行了点评,并对研究设计、研究结果及其意义进行了肯定。Kim教授认为该研究设计严谨,以对比组织检测为基础,肯定了 BENEFIT血液结果与组织的一致性,以及检测的敏感性、特异性、疗效及生存预测的可靠性。她认为该研究第一次前瞻性证实了外周血ctDNA检测EGFR突变预测一代EGFR-TKI疗效的可行性,为外周血检测EGFR突变指导一线EGFR-TKI治疗提供了更高级别的循证医学证据。同时,也提出了针对进一步分子检测的三个建议,即T790M突变的血浆检测平台的进一步探索;NGS在吉非替尼治疗疾病进展时留取血液或组织标本进行多基因分析;以及利用ddPCR对EGFR敏感性突变和T790M突变的动态变化进行定量分析。相信针对Kim教授的这些问题,我们都可以在BENEFIT研究即将出炉的分子标志物动态监测分析中找到答案。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TKI疗效#
77
#可行性#
71
#活检#
130
#FIT#
72
#TKI#
88
#WCLC#
82
液态活检技术越来越成熟了!
91
不错的.学习了.谢谢分享!
92