华人声音Nature:p53介导“铁死亡”抑制肿瘤进展
2015-03-23 佚名 生物谷
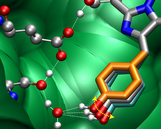
近日,细胞生物学领域著名华人科学家Wei Gu在国际期刊nature在线发表了他们的最新研究进展,他们发现经典肿瘤抑制因子p53能够通过调节细胞胱氨酸代谢以及ROS应答,介导ferroptosis过程,抑制肿瘤生长,拓展了人们对p53功能的新认识。 p53是一种肿瘤抑制基因(tumor suppressor gene),在所有恶性肿瘤中,50%以上会出现该基因的突变。p53介导的细胞周期
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
58
#肿瘤进展#
62
#抑制肿瘤#
69
#p53#
73
#华人#
69
有意思
138