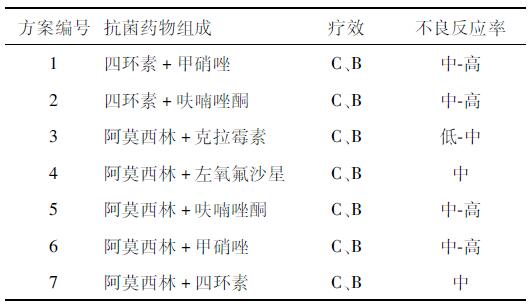
诺奖得主马歇尔:幽门螺杆菌患者不必分餐,警惕抗生素耐药性
2017-06-13 陈明明 澎湃新闻
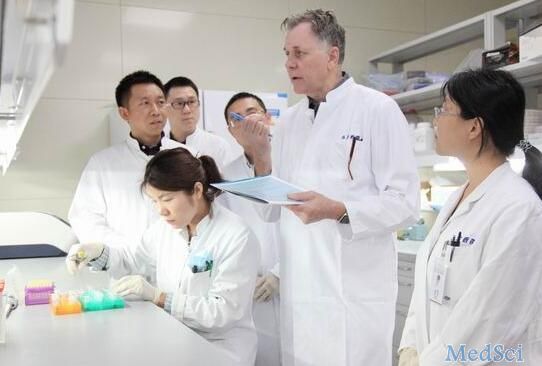
他是2005年诺贝尔生理学或医学奖得主;他提出了“幽门螺杆菌是大多数胃溃疡和胃炎的成因”这一学说;他为了验证其学说的科学性曾在1982年亲自喝下了试管里的幽门螺杆菌,不惜患上胃溃疡而后使用抗生素治愈。他,是“幽门螺杆菌之父”巴里·马歇尔教授。如今,上海市民在家门口就能让这位来自澳大利亚的专家为自己看诊。6月13日上午8时许,位于浦东即墨路的同济大学附属上海东方医院本部三楼特需门诊门口人头攒动,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#螺杆菌#
50
学习了
93
#抗生素耐药性#
64
#诺奖#
51
#抗生素耐药#
56
好文章,值得拜读,受益
89
学习了。。。。。。。。。
90
学习了新知识
90
很好,不错,以后会多学习
92
谢谢分享受益匪浅
54