European Radiology:小儿急性阑尾炎的特异性MRI表现
2021-12-28 shaosai MedSci原创
急性阑尾炎是儿童紧急腹部手术最常见的临床指征,必须与众多非手术原因的腹痛区分开来。由于儿童急性阑尾炎体征、症状和实验室检查没有特异性,临床诊断仍然具有挑战性。
急性阑尾炎是儿童紧急腹部手术最常见的临床指征,必须与众多非手术原因的腹痛区分开来。由于儿童急性阑尾炎体征、症状和实验室检查没有特异性,临床诊断仍然具有挑战性。超声波(US)、计算机断层扫描(CT)和磁共振成像(MRI)都可以提高诊断阑尾炎的准确性,但对于最佳的成像手段选择还未达成共识。
几十年来,US和CT一直是怀疑小儿阑尾炎的主要影像检查方法。然而,应用US观察阑尾受操作者经验的限制。在综合医院和专科医院,CT对儿科病人有很好的诊断效果,但患者要暴露在电离辐射中。最近有报道称,MRI在诊断小儿阑尾炎方面的表现与CT相当。美国放射学会(ACR)最新版本的适当性标准将MRI纳入主要的成像手段之一。
近日,发表在European Radiology杂志的一项研究评估了独立应用MRI特征评估小儿阑尾炎的诊断性能,为现有小儿阑尾炎MRI特定诊断标准的修正及完善提供了参考依据。
本研究评估了2014年1月至2017年12月期间因怀疑小儿阑尾炎而进行的平扫MRI检查图像。阳性诊断由手术病理或抗生素治疗后症状缓解来定义。四位儿科放射科医生在对临床数据保密的情况下,独立对研究的生物计量学进行评分。采用平衡完全区块设计来确定性能特征。
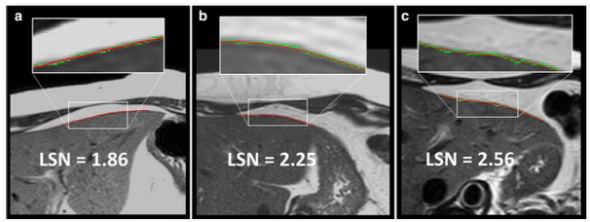
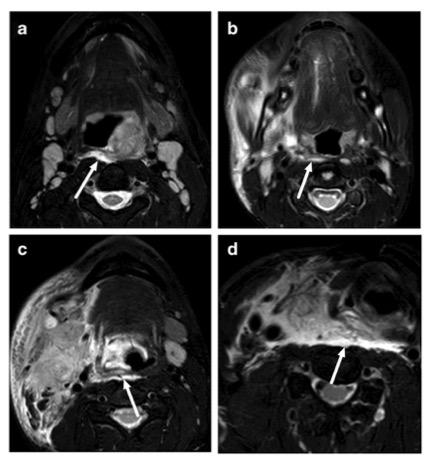
阑尾炎的总体诊断(208项研究)的敏感性为90.6%,特异性为97.7%。阳性病例的阑尾直径中位数为10.4毫米,阴性病例为5.8毫米(P < 0.001),最佳诊断截断点为7.5毫米(敏感性89.4%,特异性86.5%)。在阳性病例中,阑尾壁厚度的中位数为2.6毫米,在阴性病例中为1.7毫米(P < 0.001),最佳诊断截断值为2.3毫米(敏感性63.1%,特异性82.9%)。阑尾定性特征的表现特征包括可区分的阑尾管腔信号(敏感性89.6%,特异性83.7%)、管腔内液体信号强度(敏感性63.6%;特异性52.3%)、管腔内液体和肠壁之间的信号(敏感性91.0%;特异性37.1%)、阑尾结石(敏感性34。 9%;特异性100.0%)、腔内分层(敏感性25.9%;特异性100.0%)、阑尾壁高张力信号(敏感性31.7%;特异性100.0%)、阑尾周围液体(敏感性66.8%;特异性72.5%)、阑尾周围脂肪水肿(敏感性91.3%;特异性94.5%)和游离盆腔液体(敏感性88.5%;特异性26.0)。
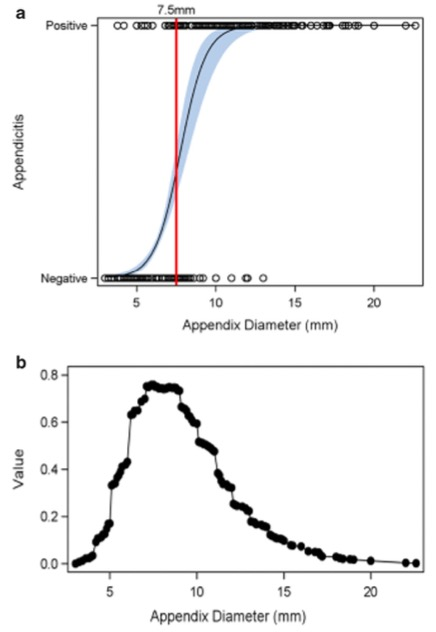
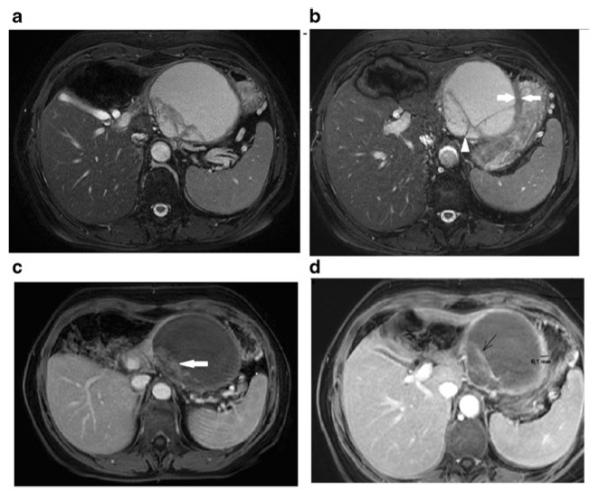
图 a图描述了阑尾炎阳性的可能性(0到100%)与阑尾直径(毫米)的关系。黑色数据点代表与阑尾直径相对应的实际阳性和阴性病例。黑色实线为斜率,代表阑尾直径与阑尾炎可能性之间的关系。浅蓝色带是围绕斜率的95%置信带。红线表示基于Youden's J指数的阑尾直径的敏感性和特异性之间的最佳阈值。 b Youden分布显示阑尾直径每增加一个单位,阳性和阴性病例之间的数学上的最佳区分。在7.5毫米时,敏感性为89.4%,特异性为86.5%。
综上所述,MRI对于评估疑似阑尾炎的儿童具有较高的敏感性、特异性和观察者之间的一致性,同时发现对识别阑尾炎最有用的个别影像特征包括:(1)阑尾周围脂肪水肿的存在,(2)直径大于7.5毫米,(3)区分阑尾管腔高强化信号和管壁信号的能力。本研究为小儿患者正常和炎症阑尾的多种生物磁共振特征提供了有价值的参考,可以协助执业的放射科医生进行准确地评估及诊断。
原文出处:Eric L Tung,Grayson L Baird,Rama S Ayyala,et al.Comparison of MRI appendix biometrics in children with and without acute appendicitis.DOI:10.1007/s00330-021-08120-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了!
89
#特异性#
75
#PE#
73
学习了#学习#
86
#急性阑尾炎#
77