盘点:心脏瓣膜置换知多少?
2016-10-25 MedSci MedSci原创
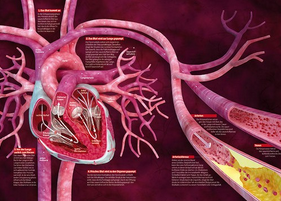
近年来,结构性心脏病经导管治疗的发展已远远超过了过去的15年。自从2000年第一代球囊扩张式瓣膜被引入血管狭窄病变治疗,新型装置、替代技术及新治疗途径已经使心脏瓣膜病治疗变得更为精准。经导管修复术与置换术使我们具备了治疗心脏入口及返流病变的能力。3D及4D成像与新技术的联合使用使治疗内容不断丰富,从术前规划到术中指导,再到术后快速评估与随访。多模态成像的应用有助于手术操作者克服各种局限性并促进
近年来,结构性心脏病经导管治疗的发展已远远超过了过去的15年。自从2000年第一代球囊扩张式瓣膜被引入血管狭窄病变治疗,新型装置、替代技术及新治疗途径已经使心脏瓣膜病治疗变得更为精准。经导管修复术与置换术使我们具备了治疗心脏入口及返流病变的能力。3D及4D成像与新技术的联合使用使治疗内容不断丰富,从术前规划到术中指导,再到术后快速评估与随访。多模态成像的应用有助于手术操作者克服各种局限性并促进多学科治疗团队的形成。这里小编整理了近期关于瓣膜置换的研究与大家分享。
【1】经导管主动脉瓣膜置换术在临床上的应用效果
由于采用经导管主动脉瓣置换(TAVR),关于其与外科主动脉瓣置换相比,临床实践效果问题已经引起了人们的关注。完整的全国性数据在调查引入的新技术是如何影响临床标准时是有用的。研究人员分析了所有进行隔离TAVR与外科主动脉瓣置换手术的数据患者的特征和在医院时的效果,这些手术都是2007年至2013年在德国进行的。
总共有32581例TAVR和55992例外科主动脉瓣置换手术进行。TAVR手术的数量从2007年的144增加至2013年的9147例,而主动脉瓣置换手术组的的数量略有下降,从8622下降到7048例。接受TAVR的患者年龄明显高于接受主动脉瓣置换患者的年龄,并有更高的术前危险。两组院内死亡率在2007年至2013年间都有所下降。中风、出血、心脏起搏器植入术(但不是急性肾损伤)的发生率也有所下降。
在2007年和2013年之间使用TAVR率显着增加;但伴随使用主动脉瓣置换手术率的下降也是比较缓慢的。接受TAVR的患者是老年人,并且比那些接受主动脉瓣置换手术的患者有更高的手术风险。两组在住院时死亡率都有所下降,但TAVR的患者下降程度更大。(文章详见——NEJM: 经导管主动脉瓣膜置换术在临床上的应用效果)
【2】主动脉狭窄中危患者,TVAR or 主动脉瓣膜置换术?
既往研究已经表明,主动脉狭窄的高危患者,经导管主动脉瓣置换术(TAVR)与主动脉瓣膜置换术的患者生存率相似。本研究旨在通过一项随机试验来评估两种方法对主动脉狭窄的中危患者的疗效。
研究共纳入了来自57个中心的2032名严重主动脉瓣狭窄的中危患者,随机分配至TAVR组或手术瓣膜置换组。初始假设是行TAVR的效果不次于手术置换。随机分配之前,基于临床和影像学表现的基础上患者进入两个队列——76.3%的患者经股动脉途径治疗,23.7%的患者经胸廓途径治疗。
结果发现,TAVR组和手术组患者的全因死亡率或致残性卒中率相当。治疗后第2年,TAVR组Kaplan–Meier事件发生率为19.3%,手术组为21.1%。经股动脉途径治疗的患者,TAVR治疗后患者的死亡率或致残性卒中率均低于手术治疗组,但是在经胸廓途径治疗的患者中,两组治疗的结果相似。手术可以减少大血管并发症少出现主动脉瓣关闭不全。与手术治疗相比,TAVR可进入较大的动脉瓣膜区域,还可以降低急性肾损伤,严重出血和新发房颤的发生率;但是手术治疗可减少大血管并发症并,可降低主动脉瓣膜反流的发生率。
总而言之,对于主动脉狭窄的中危患者来说,TAVR与手术行主动脉瓣膜置换的死亡率和卒中后残疾率相似。(文章详见——NEJM:主动脉狭窄中危患者,TVAR or 主动脉瓣膜置换术?)
【3】经导管主动脉瓣膜置换术临床获益持续可达三年
手术风险增加的严重主动脉瓣狭窄患者手术,与手术相比,经导管主动脉瓣置换(TAVR)与患者2年生存率改善相关。
研究者将由多学科中心组确认的手术风险增加的严重主动脉瓣狭窄患者,按照1:1比例随机分为TAVR组或开放手术瓣膜置换术(SAVR)组。按照程序获得这些患者3年的临床和超声心动图的结果。
结果共招募美国45个中心的797例患者,750例患者纳入研究。TAVR组患者三年全因死亡或卒中发生率显著降低。与SAVR组相比,TAVR组不良临床预后也下降,包括全因死亡率,所有卒中,和主要不良心脑血管事件。尽管TAVR组患者存在中度或重度主动脉瓣反流,但3年主动脉瓣血流动力学研究中,TAVR组优于SAVR组。两组均无瓣膜血栓形成的临床证据。
该研究发现,手术风险增加的严重主动脉瓣狭窄患者TAVR治疗后的3年临床预后优于手术组。两组间瓣膜结构的变化没有差异,但TAVR组主动脉瓣血流动力结果更有利。(文章详见——JACC:经导管主动脉瓣膜置换术临床获益持续可达三年)
【4】经导管主动脉瓣膜置换术优于手术置换
使用SAPIEN 3 经导管主动脉瓣膜置换术(TAVR),对于有严重主动脉瓣膜狭窄的中度手术死亡率风险的人群显示出了较好的30天临床预后。我们报道了对于中度危险人群使用SAPIEN 3 TAVR的长期数据,并与手术瓣膜置换进行了比较。
在SAPIEN 3 观察研究中,美国和加拿大51个中心的1077名中度危险人群被分配到接受SAPIEN 3TAVR[952 [88%] 经股动脉) ,时间为从2014年2月17日到2014年9月3日。评估了这些人群置换术后1年的全因死亡率和卒中发生率、再次干预的比例。与2011年12月23日到2013年11月6 在PARTNER 2A实验中进行手术瓣膜置换的中度危险人群的1年预后进行了比较,使用预先设定的倾向性评分分析统计两个试验基线特征的差异。
结果发现,SAPIEN 3观察研究的1年随访中,1077个接受TAVR手术的病人中79个死亡(全因死亡率7.4%;6.5%是经股动脉亚组;24人 (2%)发生卒中后残疾,6人(1%)主动脉瓣膜再次干预,13人(2%)发生中重度瓣膜旁反流。倾向性评分分析包括了963个进行SAPIEN 3 TAVR手术和747个进行手术瓣膜置换。主要复合终点的全因死亡率、卒中和中重度主动脉瓣膜反流,TAVR不劣于而且优于手术置换组。(文章详见——Lancet:经导管主动脉瓣膜置换术优于手术置换)
【5】中度危险人群的经导管VS 手术主动脉瓣膜置换术的疗效相当
先前的研究表明,高危人群主动脉瓣膜狭窄行经导管的主动脉瓣膜置换术(TAVR)与手术行瓣膜置换术的生存率相近。我们在随机试验评估了两种方法对中度危险人群的效果。
我们在57个中心,将2032名有严重动脉瓣膜狭窄的中度危险人群分配到TAVR或手术治疗组。主要终点是任何原因的死亡或卒中后2年残疾。主要假设是TAVR不劣于手术置换。在随机分配之前,病人基于临床或影像学发现进入两个队列中,76.3% 病人分配到经股动脉治疗组, 23.7% 病人分配到经胸治疗组。
结果发现,TAVR组和手术组的全因死亡率或卒中后残疾发生率相似(P=0.001 非劣效性)。2年后,Kaplan–Meier事件发生率为TAVR组19.3%,手术组 21.1%,然而经胸廓的两组治疗结果相似。TAVR可进入较大的动脉瓣膜区域,导致较低比例的急性肾衰,严重出血和新发房颤;手术组可导致较少的大血管并发症和主动脉瓣膜反流。
该研究发现,对中度危险人群,TAVR与手术行主动脉瓣膜置换的死亡和卒中后残疾的主要终点相似。(文章详见——NEJM:中度危险人群的经导管VS 手术主动脉瓣膜置换术的疗效相当)

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#心脏瓣膜#
70
#置换#
91
#瓣膜#
84
好的嘟嘟嘟额时候记得
122
好,讲的有道理
1
床位上有个胆结石的病人还可能真的要换瓣膜呢!
88
这个不错哦!
120