艾滋病合并肺结核--男性,36岁,不规则高热、咳嗽、咳痰、胸闷、气促、...
2012-02-17 贺素典,郭继丰 云南省红河州疾控中心结防
艾滋病是目前结核感染的最重要危险因素,也是防治结核的重要环节;其他可引起免疫下降的疾病,如糖尿病或激素治疗等,也是结核感染的危险因素;年龄也被考虑为独立的危险因素之一,除了接触史较长外,还可能与免疫力低下有关。肺结核诊断通常是胸片发现可疑,结合临床表现,如咳嗽嗽(超过3周)、咯血、胸痛或呼吸困难,有不明原因性发热或结核菌素试验阳性;成人锁骨上方或后方出现结节性渗出表现(经典部位,多在肺尖部)。高度
艾滋病是目前结核感染的最重要危险因素,也是防治结核的重要环节;其他可引起免疫下降的疾病,如糖尿病或激素治疗等,也是结核感染的危险因素;年龄也被考虑为独立的危险因素之一,除了接触史较长外,还可能与免疫力低下有关。肺结核诊断通常是胸片发现可疑,结合临床表现,如咳嗽嗽(超过3周)、咯血、胸痛或呼吸困难,有不明原因性发热或结核菌素试验阳性;成人锁骨上方或后方出现结节性渗出表现(经典部位,多在肺尖部)。高度提示继发性结核的可能:肺中部或下部出现渗出病灶,若症状高度可疑或有接触史,也应高度怀疑。
【病例资料】
患者,男性,36岁,不规则高热、咳嗽、咳痰、胸闷、气促、顽固性腹泻、消瘦、淋巴结肿大、腹膜后淋巴结肿大、肝大、脾大、双侧胸腔积液、心包积液等。实验室检查:贫血(Hb 60-91g/L),WBC 3.7x109/L,淋巴细胞均降低(0.16x109/L -0.40x109/L)。痰涂片检查:阴性,CD4记数69/mm3,大便潜血阳性。影像学检查:胸片表现为肺部可见大小不等粟粒状阴影。部分较均匀,部分粟粒影融合。CT表现为双肺弥漫性分布小结节影、不均匀,大小不等,l~5 mm,片状融合实变影或纵隔淋巴结肿大(图1)。发热,腹股沟淋巴结肿大,Anti-HIV(+),确证实验(+)。 入院诊断:①艾滋病;②肺孢子虫肺炎;③结核病。治疗:①抗结核治疗;②抗病毒治疗。治疗药物:异烟肼(H)、阿米卡星(A)、利福平(R)、利福喷汀(L)、乙胺丁醇(E)、对氨基水杨酸钠(PAS)、吡嗪酰胺(Z)及链霉素(S)。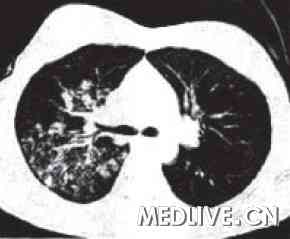
图1 患者肺部CT片
化疗方案:①2HRZE/4HR,强化期2个月,H、R、Z、E每日1次;继续期4个月,H、R每日1次。②H2H3R3Z3E3/4H3R3,强化期2个月,H、R、Z、E隔日1次;继续期4个月,H、R隔日1次。服药4个月症状消失,疗程结束,患者治愈。患者第二次发病时查:WBC 6.9x109/L。痰涂片检查:阴性,CD4记数49/mm3。服药7个月后,复查胸片,胸片异常较就诊时加重,服药8个月又出现发热,胸片异常。抗结核治疗1周,效果不佳。建议到上一级医院住院治疗。
追问病史:患者第一次发病时服用SMZ 1周,服用预防量,出现不良反应停药。随访时患者死亡。
【讨论】
HIV患者体内的结核杆菌对常规的抗结核药物反应良好。但多重耐药结核除外,因为抗耐药结核的药物通常毒性较大,而且效果较差。建议选用敏感药物,疗程持续6-9个月;若治疗前痰培养连续3次均为阴性。可将疗程缩短至6个月;若治疗2个月后,培养仍为阳性,需治疗9个月。
1、预防:
艾滋病患者不是必须进行结核病的化学药物预防。当患者的CD4+T淋巴细胞计数<200/mm3时可进行预防性化疗。其方案是:①异烟肼+利福喷汀,连续服用4—6个月。②异烟肼,连续服用12个月。预防艾滋病患者不是必须进行非结核分支杆菌病的化学药物预防,当CD4+T淋巴细胞<50/mm3时,可进行预防性治疗。以减少发生播散性鸟分支杆菌感染的概率。方案是克拉霉素每次500 mg,每日2次;或阿奇霉素每次l 200 mg,每周1次。如患者经HAART治疗使CD4+T淋巴细胞增加到>100/mm3并持续6个月以上时。可停止预防用药。 2、本组患者死亡原因分析: (1)致死原因是在抗结核治疗2个月。加抗病毒治疗(SMZ加大剂量,用治疗量)。 (2)此患者2005年出现腹股沟淋巴结肿大,伴有发热。抗结核治疗4个月,症状消失。第二次发病出现胸片异常,发热。抗结核治疗8个月,效果不好,第二次发热,应考虑做血气/氧分压检查,若PO2<70 mmHg,考虑有无缺氧,低氧血症。若有明显的喘憋,加激素治疗,逐渐减量。第二次发病同意诊断为肺孢子虫肺炎,应该再次询问有无视力模糊,进一步做眼底检查,询问有无意识障碍,考虑有无艾滋病的神经系统感染等。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











Kewl you souhld come up with that. Excellent!
209
不成功的患者资料
187
#结核#
62
#胸闷#
59
#咳痰#
81