“质子重离子医院可定向爆破肿瘤”是怎么回事?
2015-05-18 sheldon等 果壳网
被称为“治癌利器”的质子重离子技术到底是如何治疗癌症的?“定向爆破肿瘤”又是怎么回事?“定向爆破”有一定根据,但稍显夸张。恶性肿瘤治疗有三种传统疗法,手术,化疗和放疗。放疗就是用一定能量的放射线去杀灭肿瘤细胞。常见的治疗用放射线包括X射线,γ射线,电子线;不太常见的放射线包括质子,中子或重离子(例如碳离子)等等。射线没长眼睛,它既有可能杀伤肿瘤细胞,也有可能杀伤正常细胞。不过相比正常细胞,
被称为“治癌利器”的质子重离子技术到底是如何治疗癌症的?“定向爆破肿瘤”又是怎么回事?
“定向爆破”有一定根据,但稍显夸张。
恶性肿瘤治疗有三种传统疗法,手术,化疗和放疗。放疗就是用一定能量的放射线去杀灭肿瘤细胞。常见的治疗用放射线包括X射线,γ射线,电子线;不太常见的放射线包括质子,中子或重离子(例如碳离子)等等。
射线没长眼睛,它既有可能杀伤肿瘤细胞,也有可能杀伤正常细胞。不过相比正常细胞,某些类型的肿瘤细胞对射线损伤更敏感,所以从理论上讲,对患有这样的患者实施放疗就有机会控制肿瘤进展,或者根除肿瘤。因此,医生会要求放疗技术人员设法将射线能量汇聚在需要照射的肿瘤部分,尽量避开需要受保护的正常组织。
不同种类、不同能谱的射线进入人体之后,能量的沉积规律是不同的。我们以最常见的X射线和新闻中的质子射线为例进行对比。
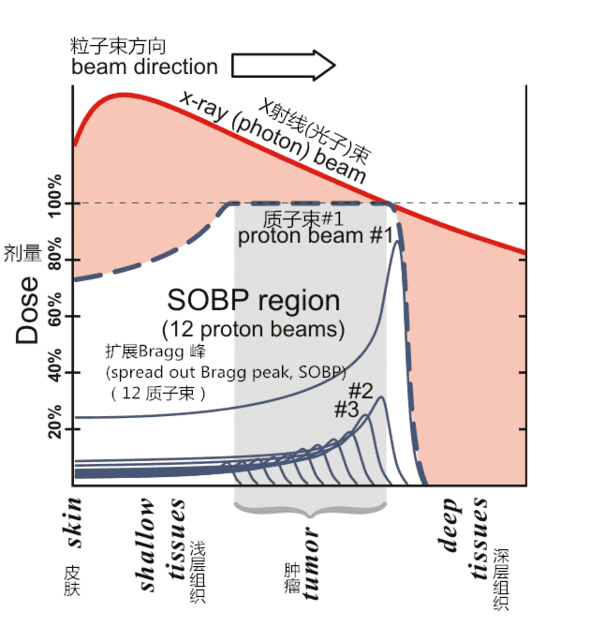
(图译自wikipedia)
假设这张图是一位患者身体的横截面。最左边是他的皮肤,浅层组织,肿瘤,然后是深层组织,直至身体的另一侧组织和皮肤(图片未画出)。有一束X射线(棕红色实线)从左边进入皮肤,像爬了一个小坡,然后逐渐跌落。这条实线的高和低分别表示X射线进入人体后的能量沉积(也就是辐射剂量)的多和少。以坡顶的能量沉积为100%的话,那么越深入人体,它的能量沉积越少。这个很容易理解,因为X射线就是一大堆高能光子(通常是MeV级),它们进入人体之后跟人体中的电子发生相互作用,走得越远消耗的光子数量越多,所以沉积的能量越少。
单看一个X射线射束的话,它的能量沉积很不合理。为了给深部肿瘤以足够的照射剂量,似乎还得先向浅层组织施加更高的剂量。在实际的放疗中,技术人员通常会在患者的不同方向设置多个X射线射束,尽可能将能量“汇聚”到肿瘤区域,保护正常组织。
再看质子射线(写有#1的细实线)。质子就是氢原子的原子核,是带正电的,这跟中性的光子有本质不同。质子进入人体后遵循完全不同的能量沉积规律,简言之就是像股市一样一路爬坡,爬到顶峰时突然断崖式下跌,跌完为止。这是因为单个质子不像光子那样,在一次碰撞中把能量全部传递出去,而是碰撞一次,传递一点儿,然后速度降低一点儿。当一定初速度的质子束达到人体的某个深度时,速度已经降低很多,实在跑不动了,于是破罐子破摔,一下子把剩余的能量全部传递出去,就形成了一个陡峭的山峰,叫做布喇格峰(Bragg Peak)。
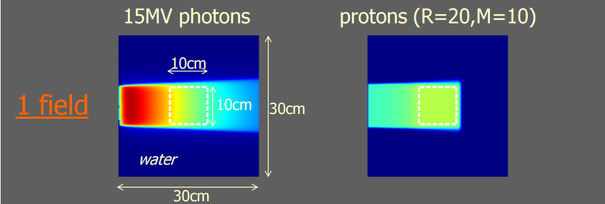
(图自美国医学物理学会资料,左为15MV X射线,右为质子束的剂量分布)
从能量沉积的角度来看,单能量质子束的“性价比”要比X射线(MeV级高能光子)要高。但为了覆盖肿区域,技术人员会考虑同一方向上用不同能量(不同初速度)的多个质子束联合照射,调制出图中粗虚线所示的高原悬崖区域。与X射线相比,这种布喇格峰延展了的质子射束的性价比还是高一些。这就是新闻中夸张地宣称质子(以及重离子)放射治疗能“定向爆破”肿瘤的物理基础。

在实际治疗中,技术人员往往会从多个角度对同一肿瘤病灶照射。在类似的多角度照射方案中,与X射线相比,质子束治疗不但更好地保护浅层组织,还能完全避免照射深层组织。这在实际治疗中有非常重要的意义。
质子束治疗还有一个特殊之处,它会让受照人体区域中的一部分本来没有放射性的原子带上放射性(主要是正电子射线,半衰期很短)。在正常治疗中,带有放射性的人体区域不会对患者本人造成大剂量的照射,但却可以帮助技术人员验证治疗计划的实施效果。用PET/CT扫描受照人体区域,得到放射性原子的强度分布,就可以重建患者在质子治疗中的实际受照情况,为下一步治疗提供依据。这在X射线治疗中是无法直接做到的。
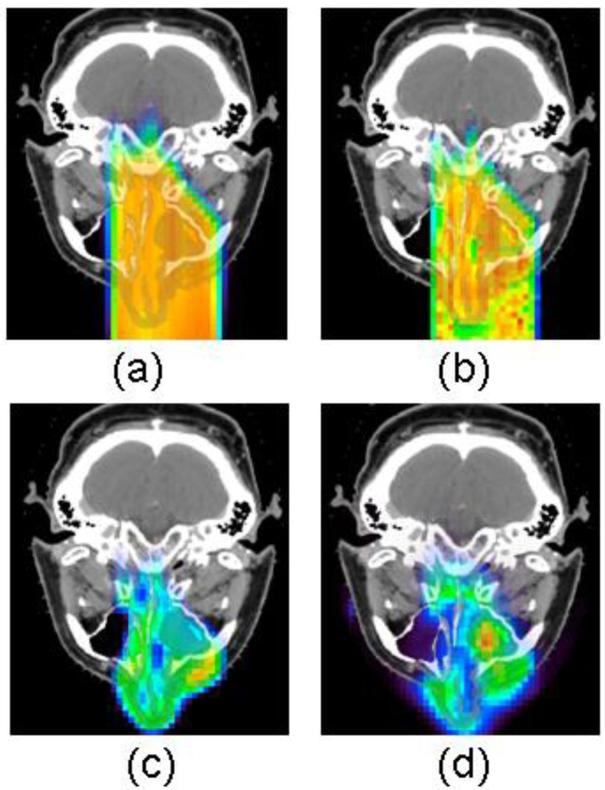
(图自美国国立卫生研究院的一篇研究论文。a 是治疗计划模拟的剂量分布;b 是用蒙特卡洛方法重新计算的治疗计划剂量分布;c 是用蒙特卡洛方法计算患者治疗后的放射性强度分布;d 是患者治疗后2分钟进行的PET/CT扫描得到的实际放射性强度分布)
精确制导导弹并不能完全替代普通炮弹,质子治疗也是如此。一个重要的原因是贵。据《放射治疗和肿瘤学》的一篇论文,质子治疗设施和X射线治疗设施的平均造价分别是9500万美元和2300万美元;每年的成本投入是2500万美元和960万美元;单次治疗的收费是740美元和230美元(一个疗程通常是20-30次治疗)。
《绝命毒师》里的老白得了晚期肺癌,接受的正是普通的X射线治疗。他在剧中因为缺少治疗费用并且对生活绝望而走向了犯罪道路,如果他接受的是质子射线治疗,不知道编剧又会搞出什么狗血情节来。
另外一个原因是质子治疗虽然在物理特性上优于X射线,但对某些恶性肿瘤某些分期的实际治疗效果上并没有想象的那么突出。例如,据《放射治疗和肿瘤学》的一篇荟萃分析论文,在I期不可手术的非小细胞肺癌患者(老白是III期或IV期)中,两种不同的X射线治疗方案的5年生存率分别是20%和42%,而质子和碳离子治疗方案的5年生存率分别是40%和42%(作者称病例人数太少,不足以下结论)。
究竟哪些恶性肿瘤哪些分期适合质子或重离子治疗,恐怕学术界还在研究之中。著名肿瘤治疗机构MD Anderson的资料称,实体的、有确定边界的、尚未扩散的肿瘤会从质子治疗中获益。自2006年起,他们用质子射线治疗了数千例肺癌、鼻咽癌、脑癌、前列腺癌和其他类型的癌症患者。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#定向#
68
#重离子#
62
还是看不懂
159
#质子重离子#
66
#质子重离子医院#
70
希望不是梦
120
夸张了
132