JCEM:新型AMPK激活/mTOR拮抗剂抑制甲状腺癌生长
2015-05-27 沐晴 MedSci原创
活化的AMPK是调节细胞内能量稳态的关键调节因子,研究认为,AMPK可通过抑制mTOR/p70S6K信号途径,抑制肿瘤细胞的生长。激活AMPK的药物,如二甲双胍和AICAR,在体内和体外实验中,都证明可以抑制甲状腺癌细胞的生长。<span lang="EN-US" style="mso-bidi-font-size:10.5pt;font-family:Frutiger-Roman; mso-b
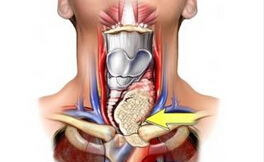
活化的AMPK是调节细胞内能量稳态的关键调节因子,研究认为,AMPK可通过抑制mTOR/p70S6K信号途径,抑制肿瘤细胞的生长。激活AMPK的药物,如二甲双胍和AICAR,在体内和体外实验中,都证明可以抑制甲状腺癌细胞的生长。OSU-53是近来研发的AMPK激活剂,体内和体外实验研究证明,OSU-53可以抑制侵袭性乳腺癌细胞的生长。
近来,有研究试图通过体外细胞研究,证明OSU-53对甲状腺癌细胞的治疗作用。研究者通过选择性基因敲除AMPK,分别检测OSU-53对甲状腺癌细胞生长、致癌信号系统、凋亡、自噬的影响。结果显示:OSU-53可以抑制体外7种甲状腺癌细胞的生长,同时激活AMPK。存在RAS或者BRAF突变的细胞系,与缺乏抑癌基因和RET/PTC1突变相比,对于OSU-53治疗更敏感,这证明OSU-53是非常强的激活AMPK,抑制mTOR信号系统,同时激活细胞自噬的药物。在选择性的敲除AMPK后,并没有观察到甲状腺癌细胞可以免于OSU-53的“杀害”。研究者发现,OSU-53还可以通过直接抑制mTOR信号途径抑制甲状腺癌细胞的生长。此外,激活RAS或者BRAF突变,可以提高细胞的自噬水平。
最终,研究者得出结论,OSU-53是一种新型的激活AMPK/拮抗mTOR的抗癌药物,可以有效的抑制多种甲状腺癌的生长,而且,在存在RAS或者BRAF突变的细胞系中作用最强。
原始出处:
al.A Novel Dual AMPK Activator/mTOR Inhibitor Inhibits Thyroid Cancer Cell Growth. J Clin Endocrinol Metab. 2015 May;100(5):E748-56. doi:10.1210
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCEM#
59
#JCE#
0
看看
166
转化吧
195
#拮抗剂#
80