刀鞘样气管
Saber-Sheath Trachea
-
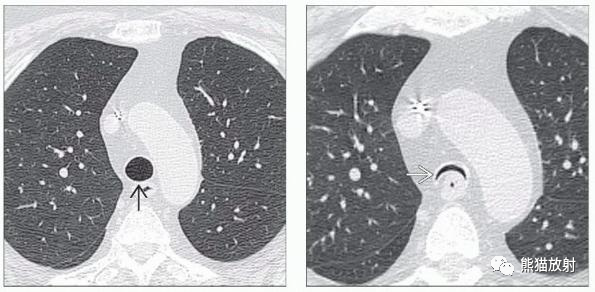
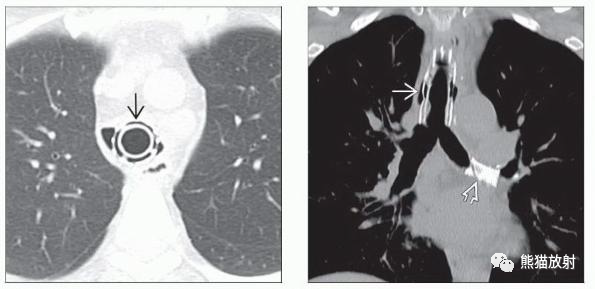
胸内气管形态异常,冠状径≤2/3矢状径
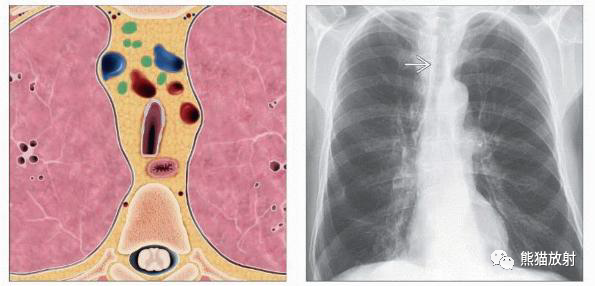
(左) 胸腔内气管形态异常,冠状径变窄,矢状径增宽。形状和形态是刀鞘样气管的特征性表现。
(右) PA胸片显示胸内气管局部狭窄。该患者肺气肿和慢性阻塞性肺疾病 (COPD),注意肺过度扩张和透亮度增高。
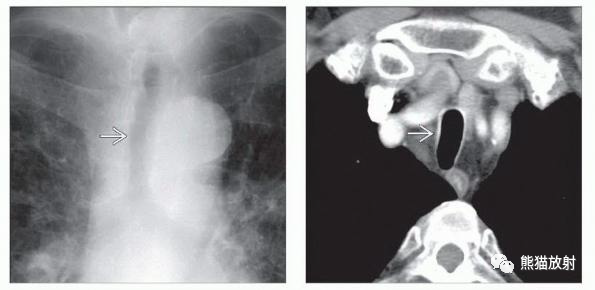
(左) 胸片显示胸腔内气管冠状径变窄,形成特征性的 “刀鞘样”形态。
(右) 同一患者的轴位CT显示胸内气管左右径变窄。刀鞘样气管患者在呼气时或Valsalva动作时可看到气管侧壁向内弯曲。
气管狭窄
Tracheal Stenosis
-
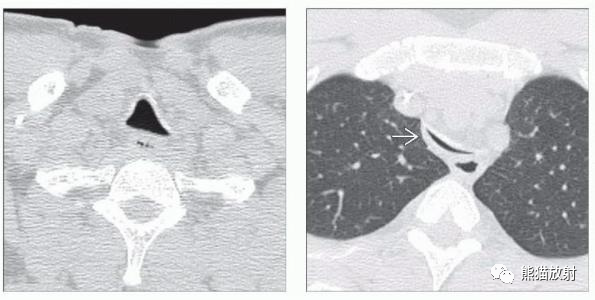
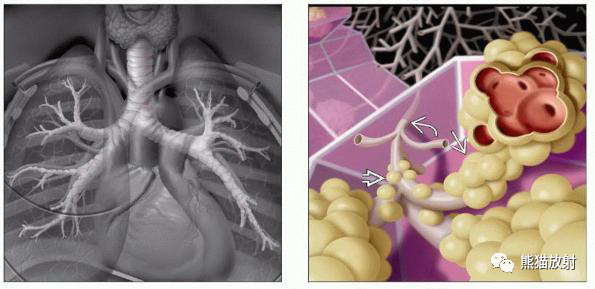
局部或弥漫性气管腔变窄
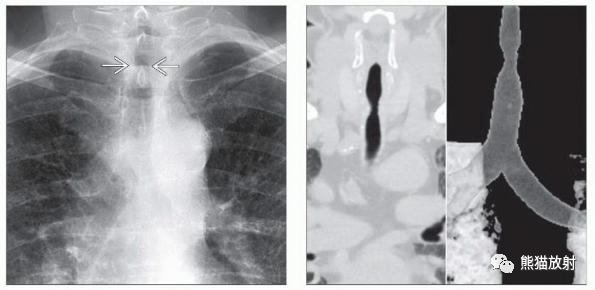
(左) 51岁男性,气管插管后狭窄。PA胸片显示气管上部局灶性短节段狭窄。
(右) 同一患者,冠状CT 和VR显示局灶性气管狭窄,具有特征性的沙漏状。气管狭窄的位置、严重程度和移行边缘是分类和临床处理的重要指标。
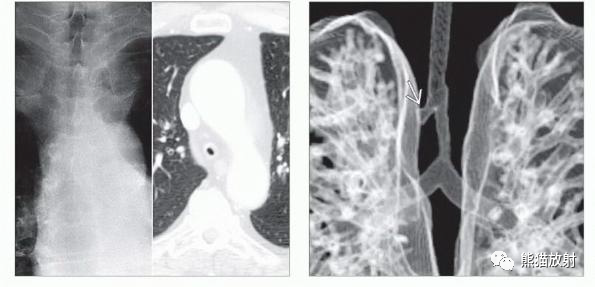
(左) 67岁复发性多软骨炎患者,PA胸片和轴位CECT图像显示弥漫性重度气管狭窄。呼气相可能对评估相关气管软化很重要。
(右) 一例肺动脉吊带患者的冠状容积CT重建显示远端气管狭窄和支气管桥。CECT可能有助于确定血管压迫或评估血管解剖,为手术做准备。
备注:有关肺动脉吊带与支气管桥的概念和关系,请点击查看(气管支气管分支异常丨基于肺叶的分类方案)
气管支气管软化症
Tracheobronchomalacia
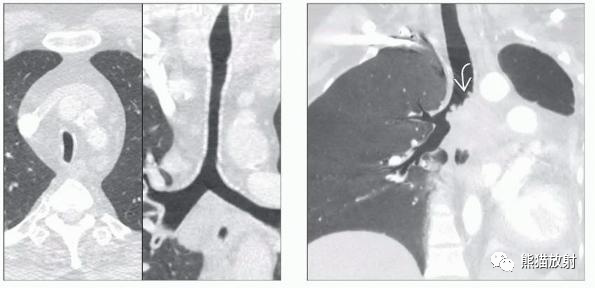
呼吸道管腔纵行弹性纤维萎缩或气道软骨结构被破坏导致的管腔塌陷、狭窄的一种病理现象。
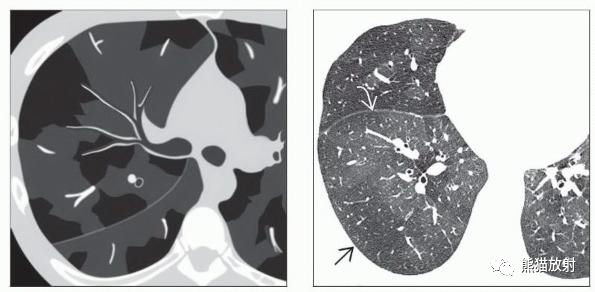
(左) 完全吸气时的轴位CT显示气管直径正常。气管后壁 (主要由气管肌组成) 向外弓,这表明这是一个吸气图像。
(右) 完全呼气时,气管严重狭窄,呈 “皱眉” 征 (气管腔新月形狭窄,类似皱眉),高度提示气管软化。吸气CT对气管软化的显示不敏感。
(左) 呼气时轴位CT显示胸外气管正常。
(右)同一患者,显示呼气时胸内气管明显狭窄,高度提示气管软化。胸外气管不受呼吸压力变化的影响。
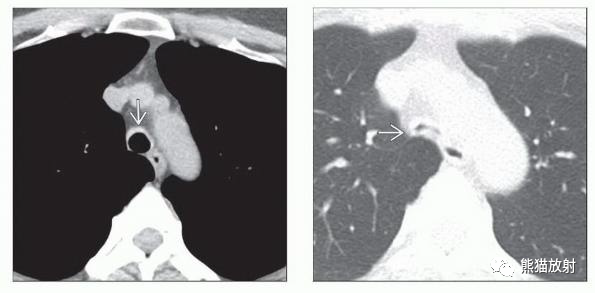
(左) 复发性多软骨炎, 轴位CT显示气管前壁增厚。与复发性多软骨炎的典型病例一样,气管后壁得以保留,因为这部分管壁中没有软骨。
(右) 同一患者,呼气相轴位CT显示气管明显塌陷,高度提示气管软化。复发性多软骨炎是气管支气管软化症的一个很重要的原因。
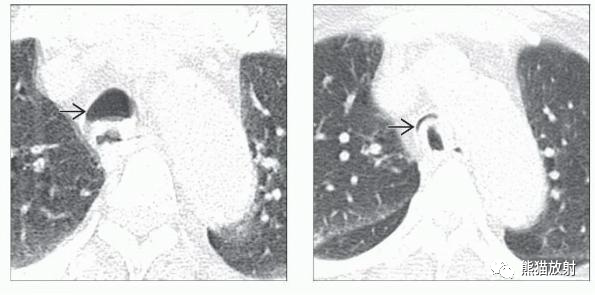
(左) 呼气末轴位CT显示气管径正常。
(右) 同一患者动态呼气时轴位CT显示气管严重塌陷,并伴有气管后壁向前弯曲,与气管软化高度一致。在诊断气管支气管软化方面,动态呼气CT比呼气末CT更敏感。
(左) 气管支气管软化病史的患者,CT显示气管内支架植入。
(右) 同一患者,冠状CT显示气管和左主支气管可见支架,用于治疗气管支气管软化。当患者禁忌或拒绝手术时,支架对改善气管支气管软化患者的症状更有价值。
气道疾病:相关解剖及病变
(左) 大气道的解剖结构。气管分叉成左、右主支气管,后者依次分支成叶、段和亚段支气管,当支气管向肺外周走行时,这些支气管继续分支并逐渐变细。气管、支气管和细支气管是传导气道。
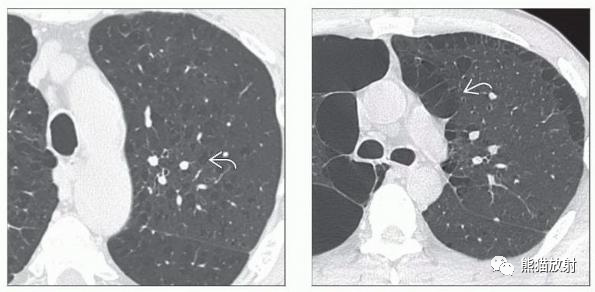
(右) 次级肺小叶的小气道:终末(弯箭)和呼吸性(空箭)细支气管以及通向肺泡囊和肺泡的肺泡管(直箭)。
(左) COPD患者,轴位和冠状位CT显示胸内气管管腔冠状变窄,胸外气管口径正常,中央气管刀鞘样气管特征。刀鞘样气管是气管狭窄的常见原因。
(右) 气管腺样囊性癌,冠状CT MinIP图像显示气管腔内有分叶状肿块,导致严重的左肺肺不张。
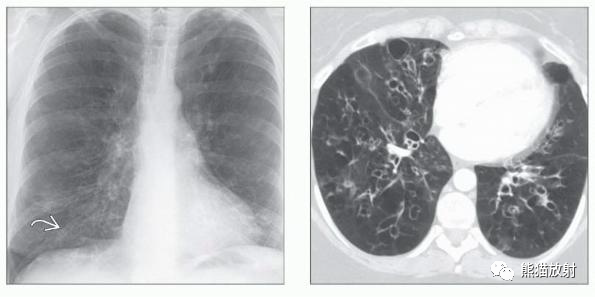
(左) 年轻女性,从小反复呼吸道感染。PA胸片显示支气管扩张的特征性影像学表现,表现为轨道征,代表扩张的支气管壁增厚。
(右) 同一患者轴位CT显示严重的双侧支气管扩张,支气管壁增厚,粘液栓塞,肺实质马赛克征。对患者进行评估并诊断为IgA缺乏症。
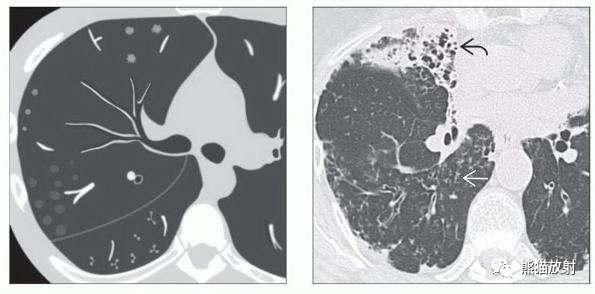
(左) 轴位NECT显示小叶中心型肺气肿,表现为低衰减的多灶性小叶中心病灶,壁难以察觉,具有代表小叶动脉的特征性中心 “点状” 结构。小叶中心型肺气肿是胸部CT常见的偶然发现。
(右) 轴位NECT显示间隔旁型气肿,表现为大小不等的小胸膜下 “囊性” 间隙,由完整的小叶间隔隔开。
(左) 细支气管炎的CT表现,其特征是小叶中心软组织和磨玻璃结节影,以及分支和树芽征,发生在邻近胸膜5-10mm处。
(右) 一例非结核分枝杆菌感染患者的轴位CT显示多灶性小叶中心结节和树芽征,另可见支气管壁增厚、中叶体积缩小和支气管扩张。
(左) 典型的马赛克征,特征是异常的低密度区与高密度区相邻。
(右) 1例移植物抗宿主病继发缩窄性细支气管炎患者的轴位CT显示马赛克征,异常高透光肺区邻近正常高密度肺实质区。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#支气管#
76
非常棒
70
#影像诊断#
89
谢谢分享
80
内容丰富,很明了
102