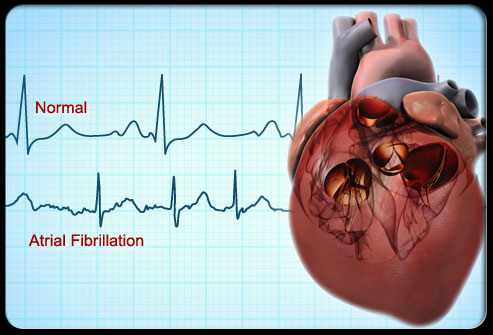
心房颤动(房颤)是一种极为常见的心律失常。全世界范围内约3200万房颤患者,美国约500万房颤患者。35~59岁的中国人群中房颤患病率为0.42%,大于60岁的中国人群中房颤患病率为1.83%。房颤是造成卒中、充血性心力衰竭、全因死亡的重要危险因素。
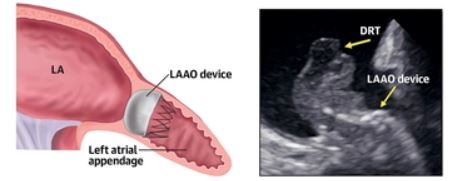
左心耳是卒中最主要的来源。左心耳形状、肌小梁走行、梳状肌形状、房颤相关的炎症水平、心房重构以及血液高凝状态,都与血栓形成有关。目前,口服华法林或其他新型抗凝药物是CHA2DS2-VASc评分≥2分患者防止卒中以及系统性栓塞的方案之一。
很多患者因为高出血风险、依从性差、药物相互作用以及经济问题,会基本或者完全放弃抗凝治疗。目前,内科经皮左心耳封堵术(LAAO)作为一种安全而有效的手段,可以替代抗凝药物预防房颤患者卒中及系统性栓塞。除防止卒中外,还可有效改善心房重构,稳定内稳态。
PLAATO封堵器(美国Appriva Medical 公司)是首个经皮左心耳封堵装置,但是该封堵器的灵活性明显落后于Watchman、ACP封堵器。作为经皮左心耳封堵术最早期的封堵装置,证实了经皮左心耳封堵术的安全性和有效性,可以有效预防卒中风险。
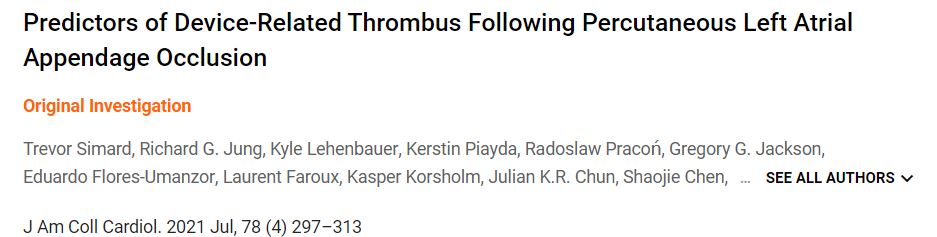
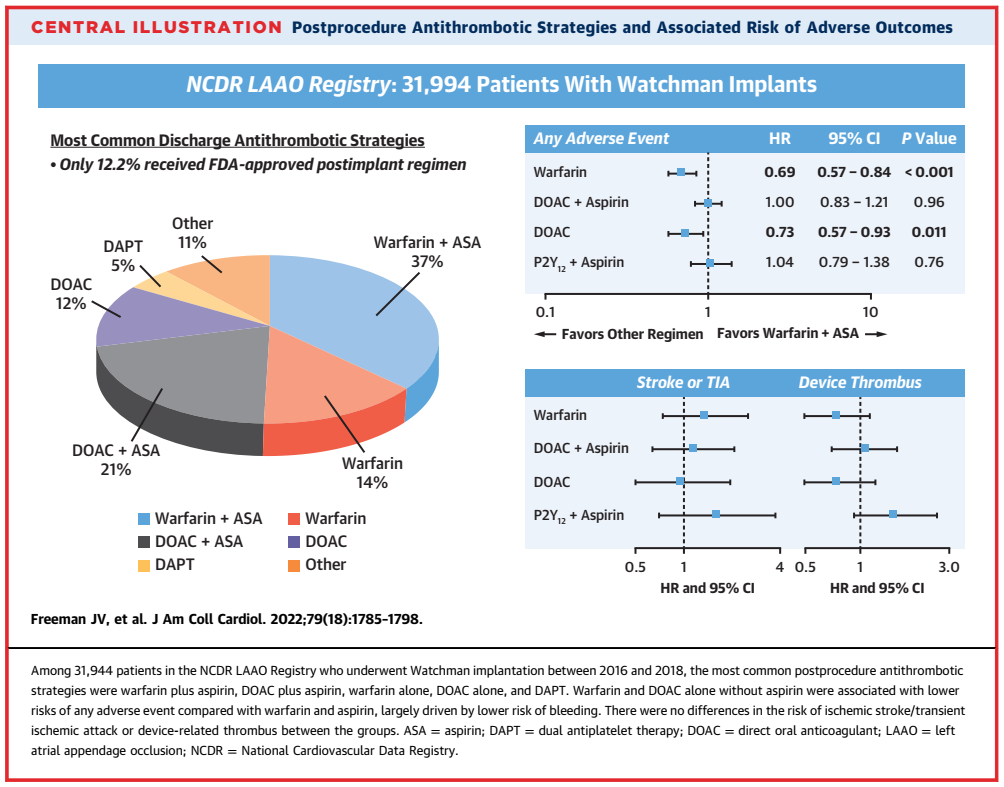
设备相关血栓(DRT)一直被认为是LAAO Achilles’的一个主要问题。然而,关于DRT预测的数据仍然有限。为此,由美国Mayo诊所牵头通过多中心合作建立了一个DRT登记处,评估DRT的结果和预测因素,结果发表在JACC上。
37个国际中心提供了有无DRT的LAAO病例(与DRT病例的设备相匹配,时间上相关)。结果共有711名患者(237名有DRT,474名无DRT)被纳入研究。DRT组和无DRT组的随访时间相似,中位数分别为1.8年(四分位数范围:0.9-3.0年)与1.6年(1.0-2.9年)。
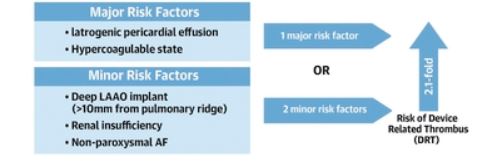
LAAO术后出现DRT的主要危险因素
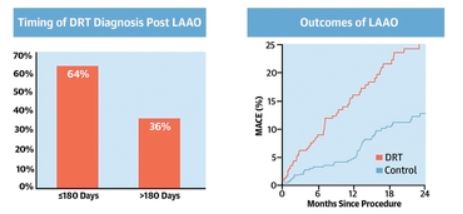
24.9%、38.8%、16.0%和20.3%的患者在0至45天、45至180天、180至365天和>365天之间检测到DRT。DRT的存在与死亡、缺血性中风或全身性栓塞的复合终点风险升高137%有关(HR=2.37;95% CI,1.58-3.56),而由缺血性中风驱动的风险则升高249%(HR=3.49;95% CI:1.35-9.00)。
多变量分析确定了5个DRT风险因素:高凝血症(OR=17.50;95%CI:3.39-90.45),心包积液(OR=13.45;95%CI:1.46-123.52),肾功能不全(OR=4. 02;95%CI:1.22-13.25),植入深度距肺静脉边缘>10毫米(OR=2.41;95%CI:1.57-3.69),和非阵发性心房颤动(OR=1.90;95%CI:1.22-2.97)。
LAAO后出现DRT的时间以及LAAO出现主要复合终点的时间
换算成危险因素积分后,与没有任何危险因素的患者相比,DRT的危险积分≥2的患者的DRT风险增加了2.1倍。此外,在最后一次已知的随访中,25.3%的患者有DRT。LAAO后的出院用药对DRT没有影响。
由此可见,LAAO后的DRT与缺血事件有关。患者和手术的特定因素与DRT的风险有关,可能有助于对转诊的LAAO患者进行风险分层。
参考文献:
Predictors of Device-Related Thrombus Following Percutaneous Left Atrial Appendage Occlusion. J Am Coll Cardiol. 2021 Jul, 78 (4) 297–313
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#封堵术#
61
#JACC#
58
#预测因素#
66
#ACC#
85
#左心耳封堵术#
184
#左心耳#
79
非常受用
81
房颤,临床上碰到很多哦
122