AJG:接受质子泵抑制剂治疗的 COVID-19 患者死亡率风险会增加
2021-06-26 MedSci原创 MedSci原创
在美国,质子泵抑制剂 (PPI) 是最常见的处方药之一,在十年内PPI的使用率从 3.9% 翻倍至 7.8%,然而大多数 (63%)服用 PPI 的患者没有胃肠道症状。
在美国,质子泵抑制剂 (PPI) 是最常见的处方药之一,在十年内PPI的使用率从 3.9% 翻倍至 7.8%,然而大多数 (63%)服用 PPI 的患者没有胃肠道 (GI) 主诉或适应症。人们越来越担心长期 PPI 使用会导致不良后果,包括社区获得性肺炎,急性/慢性肾损伤、总死亡率和肠道感染风险增加等。有研究证实COVID-19 大流行期间,PPI 暴露是与严重急性呼吸道疾病的风险增加有关,但是具体机制并不清楚。

为了对此进行更深入的研究,研究人员对住院的 2019 年冠状病毒病 (COVID-19) 患者和 COVID-19 阴性对照进行了前瞻性研究,以了解 PPI 的使用如何影响血管紧张素转换酶 2 (ACE2) 表达和粪便 SARS-CoV-2 RNA水平。然后研究人员对 2020 年3月15日至2020 年 8月15日的COVID-19 住院患者的回顾性队列进行分析,以评估 PPI 使用与死亡率的关联和死亡率的预测因素。
研究结果显示,PPI使用者的唾液ACE2 mRNA 水平高于非使用者(2.39 ± 1.15 VS 1.22 ± 0.92) ( P = 0.02)。在 694 名 COVID-19 住院患者中,PPI 使用者和非使用者的死亡率分别为 30% (68/227) 和 12.1% (53/439)。通过逻辑回归分析显示 PPI 使用([aOR] = 2.72,P < 0.001)、年龄(aOR = 1.66 每十年,P < 0.001)、种族(aOR = 3.03,P = 0.002)、癌症病史( aOR = 2.22,P = 0.008)和糖尿病(aOR = 1.95,P= 0.003)预测死亡率的危险因素。黑人患者的 PPI 相关死亡风险(aOR = 4.16,95% 置信区间:2.28-7.59)高于其他人(aOR = 1.62,95% 置信区间:0.82-3.19,P = 0.04)。
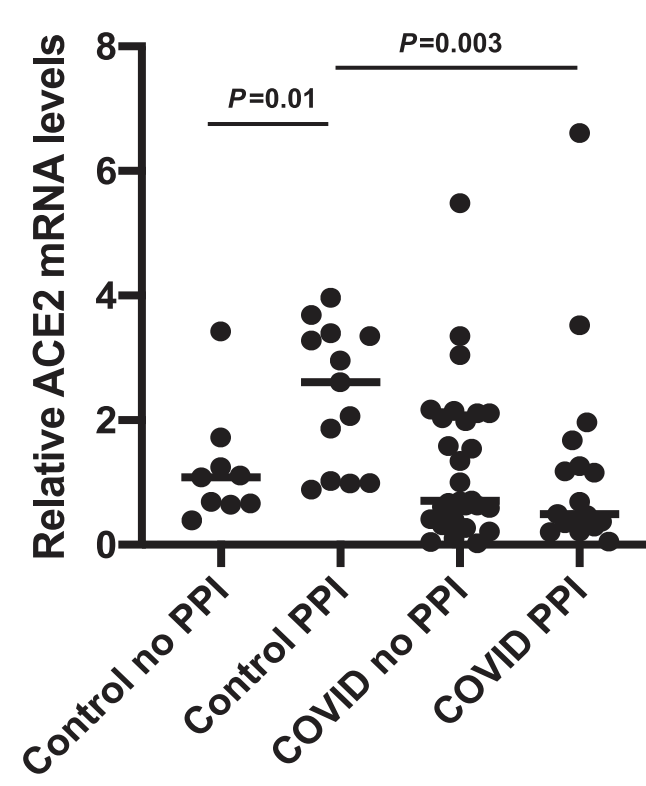
本项研究证实COVID 阴性的PPI使用者的唾液ACE2表达较高。PPI 的使用与 COVID-19 患者(尤其是非裔美国人)的死亡风险增加有关。
原始出处:
Liu, Julia J. et al. Increased ACE2 Levels and Mortality Risk of Patients With COVID-19 on Proton Pump Inhibitor Therapy. The American Journal of Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#质子泵#
104
#AJG#
60
#抑制剂#
110
抑郁症好痛苦
88
#患者死亡#
110