盘点:近期HIV相关指南共识及重大研究汇总
2016-09-28 MedSci MedSci原创
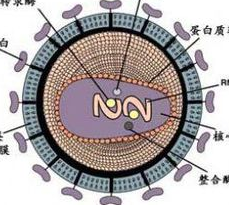
治愈HIV经常被称作HIV研究的最终梦想。虽然有效的抗HIV药物已经将艾滋病转变成了一种慢性可控的疾病,你可以携带着HIV一直生活,并且不会死于HIV感染,但终生治疗与完全治愈仍然存在很大不同,如果能找到一种既经济又能够规模化开展的HIV治愈方法,现在寻找HIV治愈方法的研究得到了越来越多的关注。这里小M整理了近期脑卒中亮点研究进展及指南共识,与大家分享。一、指南共识1、2015 BHIVA指
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#重大研究#
57
文章真好,喜欢阅读
87
好文章,长见识
65
好好学习
72
了解了!
70
学习了,分享一下!
89
继续关注!
56
谢谢分享!
35
期待能攻破此病
49
中国学者发现治疗HIV的抗体
56