支架术后照常吸烟有恶果:心脑事件增三倍
2015-10-19 壹生 壹生
对于有吸烟嗜好的冠心病患者,置入支架就万事大吉,可以美美地吸支烟?近期一项研究表示,还是戒了吧,因为对于男性急性冠状动脉综合征(ACS)患者,置入支架后吸烟是会增加术后主要不良心脑事件(MACCE)发生风险。 研究发现,术后吸烟患者MACCE的发生率是戒烟患者的3倍,不吸烟患者MACCE发生率是戒烟组的1.4倍。研究者认为这可能与戒烟可以使冠心病炎症标记物重新降低至不吸烟水平相关。
对于有吸烟嗜好的冠心病患者,置入支架就万事大吉,可以美美地吸支烟?近期一项研究表示,还是戒了吧,因为对于男性急性冠状动脉综合征(ACS)患者,置入支架后吸烟是会增加术后主要不良心脑事件(MACCE)发生风险。
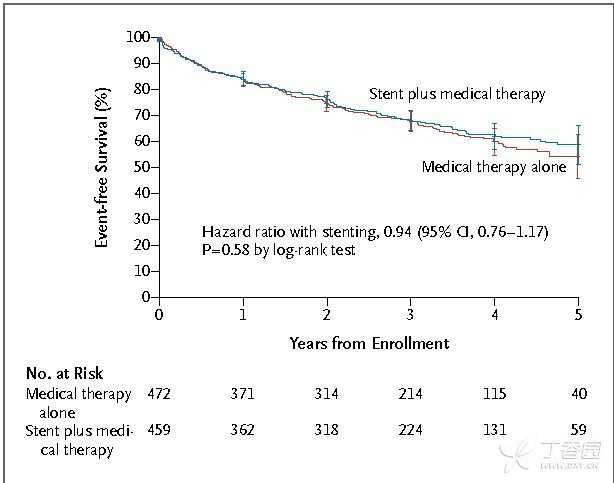
研究发现,术后吸烟患者MACCE的发生率是戒烟患者的3倍,不吸烟患者MACCE发生率是戒烟组的1.4倍。研究者认为这可能与戒烟可以使冠心病炎症标记物重新降低至不吸烟水平相关。
“所有的指南均建议一旦确诊为冠心病,应立即戒烟,但是在临床实践中,戒烟对多数患者是一种难度相当大的挑战。”研究者表示。
研究发现,这些ACS患者65.5%在术前都吸烟,虽然术后有六成吸烟患者想戒烟,,但最终仍有22.4%的人仍在吸烟。
另外,这些吸烟者多年轻,多伴有血脂异常,且文化水平较低。所有持续吸烟的患者均未服用戒烟药物。
“美国梅奥中心对5437例介入患者随访16年的研究也发现,术后继续吸烟者的MACCE发生率明显高于不吸烟组和戒烟组。从我们的研究看,这些男性患者术前术后都有较高吸烟率,在工作中应注重提高戒烟依从性。”研究者指出。
这项研究共纳入656 例接受药物洗脱支架治疗的男性 ACS 患者,根据其术后是否吸烟分为不吸烟组(n=226)、戒烟组(n=283)及目前吸烟组(n=147),平均随访27个月。
来源:刘军, 朱康宁, 朱中玉, 等. 男性急性冠状动脉综合征患者药物洗脱支架治疗后吸烟状态对临床预后的影响. 中国循环杂志, 2015,30: 631-634.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#支架术后#
0
#支架术#
75
#心脑事件#
59
~
157
赞
138
感谢分享~
126
非常感谢~
137
赞一个~
188
为了积分我也是拼了~
84