Neurology:AAN指南不建议对PFO合并卒中患者常规使用封堵设备
2016-07-28 MedSci MedSci原创
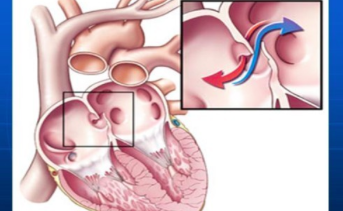
美国神经病学学会近期更新了关于卵圆孔未闭封堵装置的指南,建议这类装置不应作为缺血性卒中复发的常规预防措施。 发表在 Neurology的指南是基于近期对卵圆孔未闭(PFO)患者同时出现缺血性卒中或TIA的文献的系统回顾。研究提出了是否PFO患者关闭卵圆孔优于单独的药物治疗以及对于卒中复发预防是否抗凝治疗优于抗血小板治疗。 有限的证据 "相比其他的方法预防二次卒中,如药物减少血栓,
美国神经病学学会近期更新了关于卵圆孔未闭封堵装置的指南,建议这类装置不应作为缺血性卒中复发的常规预防措施。
发表在 Neurology的指南是基于近期对卵圆孔未闭(PFO)患者同时出现缺血性卒中或TIA的文献的系统回顾。研究提出了是否PFO患者关闭卵圆孔优于单独的药物治疗以及对于卒中复发预防是否抗凝治疗优于抗血小板治疗。
有限的证据
"相比其他的方法预防二次卒中,如药物减少血栓,仅有有限的证据支持对 [PFO] 患者使用卵圆孔封堵设备",宾夕法尼亚州大学医院神经病学副教授及实践公告联合作者Steven R. Messé 博士指出,"目前尚不清楚这些设备减少卒中风险的效果,而且这些设备与一些罕见但严重的并发症相关。"
FDA目前尚没有证据支持PFO封堵设备用于卒中预防,在美国所有此类设备的使用都是适应症之外的。
这次建议主要基于三个临床试验: CLOSURE 1, PC 和 RESPECT;以及STARFlex 设备(NMT Medical) 与Amplatzer的差异研究。基于这些试验,写作组认为尚缺乏此类设备的有效性和严重不良反应事件风险的证据,风险—益处权衡尚不清楚。
试验作者指出,尚缺乏PFO 封堵设备STARFlex 预防卒中的效果优于vs.单独药物治疗(风险差异0.13%; 95% CI, –2.2 to 2),尽管 Amplatzer设备有可能减少卒中复发风险(风险差异, –1.68%; 95% CI, –3.18 to –0.19),但有可能导致新发房颤风险 (风险差异, 1.64%; 95% CI, 0.07-3.2) 及使用后并发症风险增加 (风险差异, 3.4%; 95% CI, 2.3-5)
临床指南推荐要点:
◆临床医生应咨询患者是否要使用PFO 封堵设备,PFO 是常见的疾病,很难确定是否PFO是导致其卒中的病因,应告知他们使用设备后潜在的严重并发症风险。
◆实验目的之外,不推荐PFO 设备用于常规治疗隐源性卒中,但如果患者持续出现卒中复发,即使使用最好的药物治疗后,且未发现其他原因,则可提供Amplatzer以供选择。
◆当没有其他原因支持抗凝治疗时,临床医师应对隐源性卒中和PFO患者
常规提供抗血小板治疗,而不是抗凝治疗,因为对此类人群的抗凝治疗证据不足(风险差异,2%; 95% CI, –21 to 25)。
◆如果抗血小板治疗过程中依旧出现卒中复发,临床医师则应考虑替换抗凝治疗。
Tracey Romero指出,根据指南建议,仍需要更多的随机临床试验仔细挑选有限定的心血管风险人群及排除其他卒中病因学的患者进行研究。
原始出处:
Neurology society opposes routine use of closure devices for patients with PFO, stroke,healio,July 27, 2016
Messé S, et al.Practice advisory: Recurrent stroke with patent foramen ovale (update of practice parameter), Neurology. 2016; doi: 10.1212/WNL.0000000000002961:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#不建议#
0
常规不推荐PFO封堵治疗,且没有合并其他需要抗凝的疾病时,只需要进行抗血小板治疗即可,涨姿势
99
#卒中患者#
101
#PFO#
71
赞了,认真探究、学习。
72
文章很好,继续关注
101
#AAN#
73
#Neurol#
60