肺动脉高压特效药物万他维可能会退出中国市场,患者面临断药危机
2015-12-14 刘子晨 徐瑶 健康时报
2015年12月10日,一封由1400余名患者、医生、人大代表、病友组织、社会人士联名签署的公开信,以电子邮件的形式被发送到拜耳医药保健有限公司总部,希望其留下即将退出中国的肺动脉高压药“万他维”。 这一切源自半年前一封信。6月29日,中华慈善总会万他维患者援助项目办公室突然发出通知,终止万他维患者援助项目。通知中说,“由于捐赠方拜耳公司全球策略调整,万他维自2015年起将逐步退出中国市场”
2015年12月10日,一封由1400余名患者、医生、人大代表、病友组织、社会人士联名签署的公开信,以电子邮件的形式被发送到拜耳医药保健有限公司总部,希望其留下即将退出中国的肺动脉高压药“万他维”。
这一切源自半年前一封信。6月29日,中华慈善总会万他维患者援助项目办公室突然发出通知,终止万他维患者援助项目。通知中说,“由于捐赠方拜耳公司全球策略调整,万他维自2015年起将逐步退出中国市场”。

中华慈善总会万他维患者援助项目办公室终止援助项目通知书
对于正在接受药物援助的患者来说,援助的终止,救命药退出,意味着他们将面临更大的经济负担和断药危机。
一纸通知,救命药断了!
“我的孩子已经不在了,但我希望这种药能留下来,因为患者真的很需要它。”
6月,浙江的喻女士从当地药商处得知万他维即将断药的消息,看着家中所剩不多的药,喻女士不得不给儿子开始减药。“从一天4支到一天3支,他还没有反应。后来存药越来越少,就减到一天2支,结果身体就很快出现问题。”
儿子小虎是一名肺动脉高压患者,2014年11月起开始通过慈善项目购买万他维,同时使用安立生坦和西地那非。服药近9个月时间,病情控制得很好。喻女士告诉健康时报记者,减药后,儿子呼吸困难明显加重,早晚需要靠吸氧维持,最后连吸氧也没有效果了。本月初,29岁的小虎不幸离世。

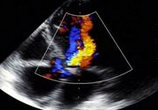
肺动脉高压患者陷入断药危机 爱稀客/供图
万他维,即吸入用伊洛前列素溶液,这是一种专门用于治疗肺动脉高压的特效药物,由拜耳医药保健有限公司(以下简称拜耳公司)生产,2006年经国家食药监局批准在国内上市。
按照正常的市场售价与使用剂量计算,用药30天,患者仅此一种药物的费用支出便达到49500元。这对任何一个家庭来说都无疑是一个巨大的灾难。
但这种情况很快便得到了改善。2008年,拜耳公司与中华慈善总会合作,共同设立了“中华慈善总会万他维患者援助项目”,实施“买一送四”的慈善援助。到2013年,赠药比例又上升到“买一送八”,这样一来,费用降到了5500元/30天,用药的人也便多了很多。
根据万他维援助项目官网的数字统计,自2008年5月份药品援助启动以来,截至2014年12月底,共计849名符合条件的肺动脉高压患者以优惠的价格,享受到了拜耳公司与中华慈善总会一起带来的爱心援助。
然而,2015年6月29日的一纸通知,使援助终止。
“如果真的出现断药,我很难想象我的病会发展成什么样。”来自江西南昌的90后女生万伟是肺动脉高压患者之一,万他维对她来说意义重大。“一用药症状就减轻,一换药病情就加重。“在病情严重的时候,短短的200米路程,万伟需要走6分钟。而用药之后,6分钟的时间则能走到360米。
他们所在病友群中,每天都会有人发出这样的声音:药快没了,我该怎么办?
天价替代药品,难解用药困境
实际上,在小虎断药的最后阶段,医生提供了另外一种替代药品:瑞莫杜林(也是一种进口药物)。这款由UNITED THERAPEUTICS CORPORATION生产的药品,与万他维同属于前列环素类似物,售价9900元一支。母亲带着小虎从浙江赶到北京阜外医院,试了三支瑞莫杜林,效果却并不明显。第二次再想去试药时,小虎身体已经虚弱得无法出门了。
阜外医院心血管内科主任医师柳志红表示,万他维自2006年进入中国市场以来救治了很多肺动脉高压患者,特别是重症患者。本来国内治疗肺动脉高压的药就少得可怜,如果万他维真的撤出,对于病人来讲确实是非常不利的,尤其是正在用药的患者。
价格上,瑞莫杜林一支9900元也让许多患者难以承受。 “现在已经花掉一座房子的钱了。”万伟告诉记者。为了攒够看病、用药的钱,万伟的父母卖掉了一套房子。父母二人都是普通的退休工人,每个月也仅有两三千块钱的退休工资。”
其实,即便是克服了价格困难,万他维的撤出仍然会对肺动脉高压的临床产生重大影响。柳志红表示,由于国内没有医用的一氧化氮,因此,肺动脉高压患者做急性血管反应实验时国内选用的主要是万他维,一旦万他维退市不仅会影响到患者的治疗,也势必影响到患者肺血管病变程度的评估以及治疗策略的抉择。
根据中华慈善总会官网数据,国内目前肺动脉高压患者1200万人。对于正在使用这款药物的患者而言,无疑并不希望万他维真的撤出中国市场。根据北京爱稀客肺动脉高压罕见病关爱中心的一项调查显示:20.8%的患者对于药物退出中国表示非常恐惧,27.7%的患者表示非常担心断药或换药会影响目前的治疗效果,22.6%的患者担心出现心衰等紧急情况时无药可用,94.9%的患者表示如万他维援助项目得以延续,便会继续使用万他维。
慈善援助与企业成本的两难
在写给拜耳公司的联名信发出后不久,国内的肺动脉高压患者组织也收到来一封来自美国肺动脉高压协会的书信声援。这同样是一封写给拜耳公司首席执行官Marijin Dekkers先生的信。信中提及,在美国并未出现万他维退市的情况,因此对在中国市场的退出行为感到十分难以接受,并尖锐提问:难道中国患者的生命比不上美国患者的生命吗?
实际上,在《关于终止万他维患者援助项目的通知》中,已经明确的表述,援助项目终止是由于“捐赠方拜耳医药保健公司全球策略的调整,万他维自2015年起将逐步退出中国市场。”就是这一内容,在引起患者强烈反对之时,也有人质疑:为何单单要退出中国市场?
一位不愿透露姓名的业内人士告知记者,企业在罕见病药物研发上投入了大量的成本,这种药进入中国,只有几百人正在使用,也没有医疗保险支持,企业撤出也情理之中。不过,也有人认为,企业撤出之前,应妥善处理好患者用药问题。
北京爱稀客肺动脉高压罕见病关爱组织透露,关于推动万他维进入医保的工作一直在进行。去年,爱稀客还联合深圳地区的专业医生向当地社保部门提供过药物有效性的相关医学资料,试图将药物先纳入深圳重大疾病医疗保障体系。
在国内,并非没有爱心援助项目成功的先例。拜耳公司所生产的血友病患者所用药物“拜科奇”在中国便以“共付机制”,通过中华慈善总会、地方慈善机构、医疗保险和患者共同承担治疗费用的模式,帮助中国甲型血友病患者获得了治疗,并取得了较好的效果。
而像中华慈善总会安维汀慈善援助项目(结直肠癌)则公开表明:如有因不可抗力或因特殊原因必须停止援助,我们会提前6个月通过多种渠道告知公众,对于已经预约成功和已经开始领药的患者,我们将保证这些患者的持续援助直至患者到达停药的标准。
在美国肺动脉高压协会给拜耳公司的信件中,便明确提出两个要求:1、对2015年7月1日起突然终止万他维慈善援助项目做出解释;2、为需要继续使用万他维的中国患者提供药物或者帮助他们过渡到其他方案,更正之前的错误决定。
一位接近拜耳公司内部的人士告诉记者,此次做出全球战略调整,确实是出于市场运行情况的考虑。关于接下来是否会有相关举措,帮助中国患者解决用药问题,或是帮助过渡到其他治理方案,记者分别致函中华慈善总会及拜耳大中华区总部,目前仍在等待回复。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#特效药#
81
#动脉高压#
69
唉…
164
应该有个中国市场…
161
不应该这样!
129
唉…
144
好文章,值得看。
142
中国是咋啦
100
总会有别的办法的
133