Br J Cancer:TARGIT-IORT(乳腺癌肿块切除术中靶向术中放疗)的随机临床试验研究
2021-05-27 xiaozeng MedSci原创
大多数的乳腺癌患者一般适合进行保乳手术和辅助放疗的治疗,而非全乳切除术。对于早期乳腺癌患者,辅助放疗的部位可能仅限于肿瘤灶位(tumour bed),且在保乳手术(肿块切除术)中可立即进行辅助治疗。因
大多数的乳腺癌患者一般适合进行保乳手术和辅助放疗的治疗,而非全乳切除术。对于早期乳腺癌患者,辅助放疗的部位可能仅限于肿瘤灶位(tumour bed),且在保乳手术(肿块切除术)中可立即进行辅助治疗。因此,研究人员提出了TARGeted术中放疗(TARGIT-IORT)的概念。
TARGIT-IORT试验旨在实现准确定位和快速形成的肿瘤灶位放疗策略,其仅集中于目标组织,使正常组织和器官(如心脏、肺、皮肤和胸壁结构)免受不必要的和具有潜在破坏性的放射治疗。
研究人员设计了TARGIT-A随机试验,报告显示,乳腺癌肿块切除术中适应风险的靶向术中放疗(TARGIT-IORT)与全乳外束放疗(EBRT)一样有效。而该研究进行了进一步的详细分析。
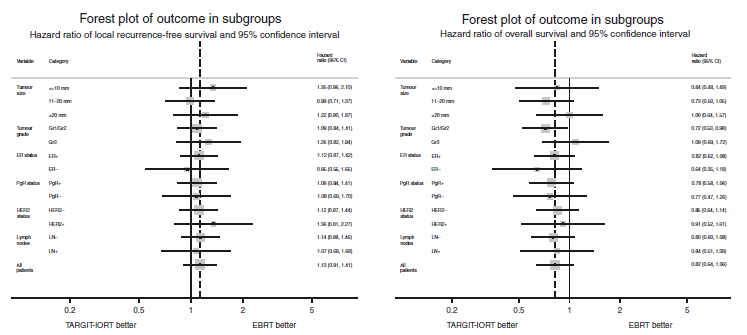
在该研究中,共招募2298名妇女(≥45岁,浸润性导管癌≤3.5cm,cN0–N1期)进行随机研究。研究人员主要调查了肿瘤大小,分级,ER、PgR、HER2水平以及淋巴结状态对患者的局部无复发生存率的影响,以及局部复发对远端复发以及患者死亡率的影响。
森林图显示肿瘤亚组的局部无复发生存率和总生存率
结果显示,在每个肿瘤亚组中,TARGIT-IORT和EBRT之间的局部无复发生存率并无差异。与EBRT组不同的是,TARGIT-IORT组的局部复发率并不是较高的远端复发率或死亡风险的预测指标。
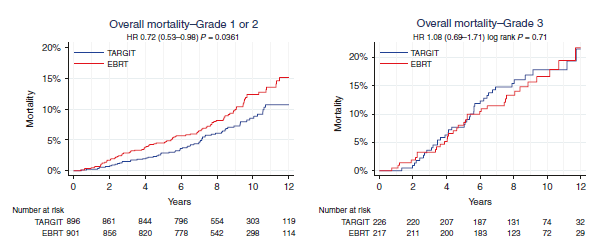
因此,研究人员建议在TARGIT-IORT治疗后推荐补充性EBRT的新预测工具。进一步的研究显示,即使在患者接受补充EBRT的情况下,TARGIT-IORT组的非乳腺癌死亡率也显著降低。
亚组分析各分级癌症患者的总生存率
总而言之,该研究结果揭示,在所有亚组中,TARGIT-IORT与EBRT治疗策略一样有效。与EBRT不同的是,TARGIT-IORT治疗后的局部复发具有较良好的预后。因此,TARGIT-IORT治疗策略可能具有潜在的治疗效果。
原始出处:
Vaidya, J.S., Bulsara, M., Baum, M. et al. New clinical and biological insights from the international TARGIT-A randomised trial of targeted intraoperative radiotherapy during lumpectomy for breast cancer. Br J Cancer (25 May 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#随机临床试验#
75
#切除术#
68
#肿块#
70
高质量研究,读起来真爽,谢谢梅斯
114