Nature & Genes&Dev & EMBO J:肠癌背后的基因错误
2015-09-11 佚名 生物谷
随着肿瘤产生发展错误就会频频出现,而且每次一旦细胞分裂产生产生两个细胞,这些错误就会发生改变而且不断变得多样化;但在某些时候早期事件引发的癌症通常会被直接发现,就拿肠道癌来说,科学界在几乎30年来都认为是一种特殊的基因引发肠癌的发生。早在20世纪80年来来自英国癌症研究中心的科学家就发现了一种名为APC的腺瘤样息肉基因的错误拷贝,而且研究者在10例肠癌患者中就发现有8名患者携带APC的

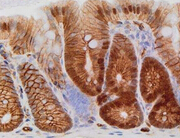
当APC错误在肠道内皮细胞中发生时就会引发接二连三的生长信号,从而促进细胞失控地复制,进而引发肠癌,而很多年来,研究者在多种疾病的研究中都肯定了APC错误的重要性。在正常的肠道细胞中,APC其中一项关键工作就是维持细胞中β连环蛋白的水平处于约束状态,一旦APC发生损伤,β连环蛋白水平就会增加,使得细胞暴露于多种生长信号中,从而细胞就会一直生长,这些信号被称为Wnt信号通路,其在肠癌的发病过程中扮演着重要角色。
肠道可以分为两部分—小肠组织和大肠组织,此前对小鼠进行研究发现,关闭肠道细胞中APC的功能就会引发小肠和大肠发生肿瘤。于是来自国外的研究人员就表示,为了观察是否APC的缺失会通过β连环蛋白来诱发肠癌,我们检测了是否工程化地含有错误的、活性版本β连环蛋白的细胞可以引发肿瘤。
研究者表示,我们在小鼠机体中测定了E-钙黏蛋白(E-cadherin)的水平,结果发现,相比小肠而言,大肠中的E-钙黏蛋白(E-cadherin)水平较高,而且E-钙黏蛋白(E-cadherin)的水平的增加的确可以帮助清理过多的β连环蛋白,从而抑制肠道中肿瘤的发生。β连环蛋白的错误在人类肠癌中并不常见,然而APC错误却在100例患者中的80例患者身上都会发生。
研究者David表示,是否改变E-钙黏蛋白的清理水平就可以帮助有效抑制肿瘤发生呢?研究者表示E-钙黏蛋白可以帮助有效抑制肠癌的发生。后期研究者们将进行更多深入的研究解析引发肠癌的分子机理,他们期望早日开发出治疗肠癌的新型个体化疗法。
原文出处:
The Cancer Genome Atlas Network.Comprehensive molecular characterization of human colon and rectal cancer. nature.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Dev#
56
#Gene#
54
这篇文章有一定深度
159
是一篇不错的文章
127
赞
156
#Nat#
62