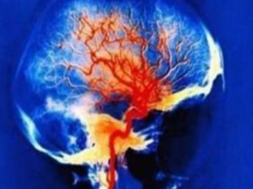
Stroke:脑出血后淋巴细胞减少症是不良预后的独立预测因子
2016-06-30 phylis 译 MedSci原创
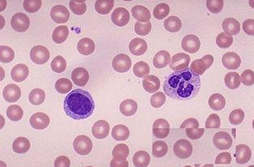
背景:卒中相关的免疫抑制越来越成为公认的感染的触发因素,从而有可能影响卒中预后。具体来说,脑出血(ICH)后淋巴细胞减少只有在小型回顾性研究混合颅内出血中报道。该研究调查淋巴细胞减少的自然过程,入院和住院期间与淋巴细胞减少症(LOA)相关的参数,并且评估脑出血患者淋巴细胞减少对临床的影响。方法:这项观察性研究包括连续855例脑出血患者。机构前瞻性数据库中获取患者的人口统计学、临床和影像学资料以及实
背景:卒中相关的免疫抑制越来越成为公认的感染的触发因素,从而有可能影响卒中预后。具体来说,脑出血(ICH)后淋巴细胞减少只有在小型回顾性研究混合颅内出血中报道。该研究调查淋巴细胞减少的自然过程,入院和住院期间与淋巴细胞减少症(LOA)相关的参数,并且评估脑出血患者淋巴细胞减少对临床的影响。
方法:这项观察性研究包括连续855例脑出血患者。机构前瞻性数据库中获取患者的人口统计学、临床和影像学资料以及实验室和住院资料。通过邮寄问卷评估3个月的功能预后。淋巴细胞减少症被定义为小于1(109/L),并且与患者的特点及预后相关。
结果:LOA的患病率为27.3%。LOA的患者与不良神经功能状态(18 [ 10-32] vs 13 [5-24 ]),血肿量大(18.5 [6.21-46.2 ] vs 12.8 [4.4-37.8 ])、不良预后相关(74.7% vs 63.3%)。住院期间淋巴细胞计数的自然病程显示,第5天淋巴细胞为最低点1.1(0.80-1.53 [ 10(9)/升])。与LOA的患者相比,第5天淋巴细胞减少的患者感染发生率增加(63 [ 71.6 ] vs 113 [ 48.5 ]),3个月预后更差(76 [ 86.4 ] vs [ 75.1,175))。校正基线混杂因素,多变量Logistic和接受者操作特征的分析显示:第5天淋巴细胞减少与不良预后相关(第5天淋巴细胞减少:OR,2.017(95%CI,1.029-3.955);LOA:OR,1.391 [ 0.795-2.432 ];ROC:第5天淋巴细胞减少:ROC= 0.673,Youden指数= 0.290;LOA:ROC= 0.513,P = 0.676,约登指数= 0.084),而接受者操作特征分析显示年龄或血肿体积与第5天淋巴细胞减少症(年龄:ROC= 0.540,P = 0.198,约登指数= 0.106;血肿体积:ROC= 0.550, Youden指数= 0.1224)不相关。
结论:ICH患者常出现淋巴细胞减少症,可能与不良功能预后相关的独立因子。淋巴细胞减少症对预后的影响甚至比LOA更大,这一发现可能为特定亚型的ICH开辟新的治疗途径。
原始出处:
Giede-Jeppe A, Bobinger T, et al. Lymphocytopenia Is an Independent Predictor of Unfavorable Functional Outcome in Spontaneous Intracerebral Hemorrhage. Stroke. 2016 May
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了,好文值得点赞!
97
#淋巴细胞#
58
#预测因子#
98
#不良预后#
55
学学学习了
152