美国胸科医师学会发布VTE抗栓治疗指南
2016-01-11 MedSci MedSci原创
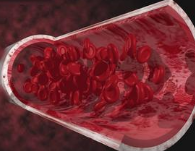
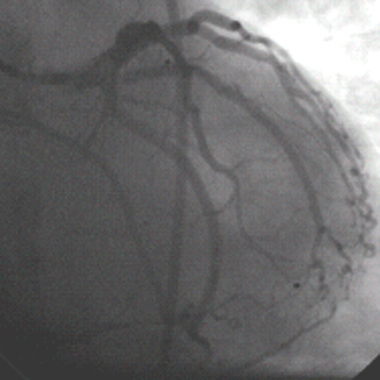
日前,美国胸科医师学会发布了静脉血栓栓塞(VTE)抗栓治疗的最新指南,包括对非维生素K拮抗剂类口服抗凝剂的使用指导。发表于《胸科》(Chest)杂志的建议最近更新或补充包括:对于腿部深静脉血栓形成(DVT)或肺栓塞(PE)的非肿瘤患者,指南建议前3个月及以后使用达比加群、利伐沙班、阿哌沙班或依度沙班,而不用维生素K拮抗剂。停止抗凝治疗的不明原因近端DVT或PE患者,如无阿司匹林禁忌,应接受阿司匹林
- 对于腿部深静脉血栓形成(DVT)或肺栓塞(PE)的非肿瘤患者,指南建议前3个月及以后使用达比加群、利伐沙班、阿哌沙班或依度沙班,而不用维生素K拮抗剂。
- 停止抗凝治疗的不明原因近端DVT或PE患者,如无阿司匹林禁忌,应接受阿司匹林来降低VTE复发风险。
- 对于腿部急性DVT患者,不推荐使用弹力袜来预防血栓形成后综合征(PTS)。然而,对于有PTS症状的患者,“往往可以试用逐级增压弹力袜”。
- PE风险低的患者可以在家接受治疗或早期出院。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










原始文章看不了!
109
亲,现在还能给我发个链接么
100
学习了,希望有更详细的
196
#治疗指南#
55
弹力袜的使用值得思考。
145
不错哦
216
有意思
121
赞一个
118
牛
165
阿司匹林降低VTE复发风险,之前指南好象没推荐
72