Cell Rep:SHP1调控间充质干细胞分化的新机制
2016-07-18 中科院上海生命科学研究院 中科院上海生命科学研究院
SHP1调控MSCs分化方向的机制。(1)SHP1促进MSCs向成骨细胞分化,并抑制向成脂分化;(2)SHP1通过增强Wnt信号进而调控MSCs的分化。具体来讲就是,SHP1去磷酸化GSK3β的Y216位点,抑制GSK3β的激酶活性,使得β-catenin得以累积,从而促进下游基因的转录。7月8日,国际学术期刊《细胞-报告》(Cell Reports)在线发表了中国科学院上海生命科学研究院/上海交
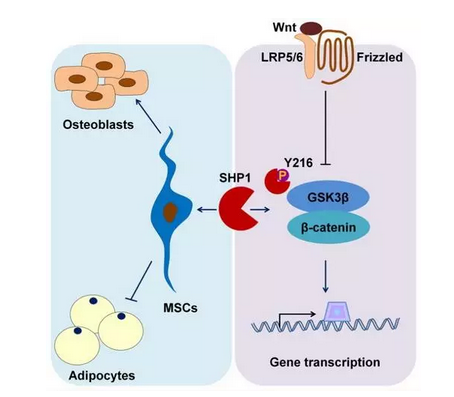
SHP1调控MSCs分化方向的机制。(1)SHP1促进MSCs向成骨细胞分化,并抑制向成脂分化;(2)SHP1通过增强Wnt信号进而调控MSCs的分化。具体来讲就是,SHP1去磷酸化GSK3β的Y216位点,抑制GSK3β的激酶活性,使得β-catenin得以累积,从而促进下游基因的转录。
7月8日,国际学术期刊《细胞-报告》(Cell Reports)在线发表了中国科学院上海生命科学研究院/上海交通大学医学院健康科学研究所时玉舫研究组题为SHP1 Regulates Bone Mass by Directing Mesenchymal Stem Cell Differentiation 的最新研究成果,揭示了蛋白酪氨酸磷酸酶SHP1调控间充质干细胞(mesenchymal stem cells,MSCs)分化的新机制。
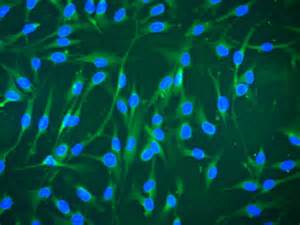
MSCs最早在骨髓中发现,是一种具有与成纤维状细胞相似形态的多能干细胞,能够分化为脂肪细胞和成骨细胞。作为骨骼和脂肪组织的共同源泉,MSCs向成脂和成骨方向的分化处于一个平衡状态,该状态的失衡与多种代谢疾病如肥胖、骨质疏松和骨硬化症等密切相关,但MSCs的成脂成骨分化的具体调节机制尚未阐明。
博士研究生蒋梦会在研究员时玉舫和王莹的指导下发现,蛋白酪氨酸磷酸酶SHP1作为细胞内信号传导的关键分子参与调控MSCs成脂成骨分化。基于SHP1突变型(mev/mev)小鼠自发骨质疏松的表型分析,研究发现SHP1突变小鼠骨髓来源的MSCs成骨分化能力显着降低,成脂分化潜能明显提高。利用SHP-1抑制剂以及siRNA敲低SHP-1在MSCs中的表达可以得到与SHP1突变小鼠骨髓来源的MSCs相似的分化现象。将MSCs与羟基磷灰石植入裸鼠后,SHP-1突变小鼠骨髓来源的MSCs骨形成明显减少,脂肪形成增加。通过一系列研究发现,SHP1对MSCs成骨成脂分化的调节依赖于其与GSK3β结合,并利用其酶活性使得GSK3β的pTyr216位点去磷酸化,从而诱导β-catenin累积促进Wnt信号,引起成骨分化的增加。利用SHP1fl/flDermo1-cre小鼠,这个研究团队进一步证明在MSCs中条件性去除SHP-1,该小鼠表现出明显的骨质减少和脂肪组织增多。该研究揭示了SHP1调控MSCs分化的新功能,并对理解骨质疏松和肥胖的形成机制具有重要意义,提供了新的视角。
该工作得到了科技部、国家自然科学基金委、中科院和上海市科委的相关资助。
原始出处:
Jiang M, Zheng C, Shou P, Li N, Cao G, Chen Q, Xu C, Du L, Yang Q, Cao J, Han Y, Li F, Cao W, Liu F, Rabson AB, Roberts AI, Xie W, Wang Y, Shi Y. SHP1 Regulates Bone Mass by Directing Mesenchymal Stem Cell Differentiation. Cell Rep. 2016 Jul 5. pii: S2211-1247(16)30775-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#间充质干细#
53
#CEL#
49
#Cell#
40
#细胞分化#
46