DDW 2016:高分辨率色素内镜监测溃疡性结肠炎显优势
2016-06-07 佚名 中国医学论坛报
在DDW2016公布的一项研究表明,在长期溃疡性结肠炎(UC)患者中,高分辨率色素内镜(CE)伴靶向活检在结肠炎相关性不典型增生病变检出方面不优于高分辨率白光内镜伴随机活检,但前者在所有不典型增生病变检出方面有改善趋势。 此项前瞻性多中心试验共纳入210例长期UC患者(广泛性结肠炎≥8年或左侧UC≥10年),并随机给予高分辨率白光内镜伴随机活检(HDWL)或高分辨率副送水功能CE伴靶向活检(HD
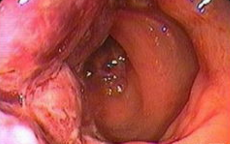
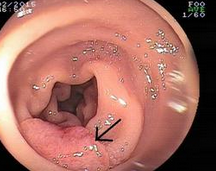
在DDW2016公布的一项研究表明,在长期溃疡性结肠炎(UC)患者中,高分辨率色素内镜(CE)伴靶向活检在结肠炎相关性不典型增生病变检出方面不优于高分辨率白光内镜伴随机活检,但前者在所有不典型增生病变检出方面有改善趋势。
此项前瞻性多中心试验共纳入210例长期UC患者(广泛性结肠炎≥8年或左侧UC≥10年),并随机给予高分辨率白光内镜伴随机活检(HDWL)或高分辨率副送水功能CE伴靶向活检(HDCE)监测。主要终点为结肠炎相关性不典型增生检出率,次要终点为包括散发腺瘤在内的所有结肠不典型增生检出率、结肠镜撤出事件以及总活检数量。
结果显示,在接受内镜监测的长期UC患者中,与HDWL相比,HDCE未能改善结肠炎相关性不典型增生病变检出率(2.9%对4.6%;P=0.722)。然而,与HDWL相比,HDCE在包括结肠炎相关性不典型增生和散发腺瘤在内的所有不典型增生检出方面有改善趋势(20.6%对12.0%;P=0.093)。HDCE操作事件与HDWL相当(17.8±7.3对18.9 ± 7.1分钟)。与HDWL相比,HDCE使总活检数量显著减少(9.2 ± 4.5对33.6 ± 10.9;P<0.001)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#高分辨率#
66
#溃疡性#
57
#色素#
71
#高分辨#
64
学习一下!
143
#内镜#
0
#DDW#
71