JCEM:血钠异常是COVID-19住院患者发病率和死亡率的预测指标
2021-02-25 MedSci原创 MedSci原创
住院期间血钠异常是COVID-19患者预后不良的危险因素,高钠血症和低钠血症分别与更大的死亡和呼吸衰竭风险相关。血钠水平可用于COVID-19患者的危险分层。
血钠异常是细菌性肺炎患者死亡率的独立预测指标。目前,缺乏新冠肺炎(COVID-19)患者血钠异常的发生率和预后影响的数据。
近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,这项回顾性纵向队列研究纳入了所有在伦敦两家医院就诊的COVID-19成年患者。研究人员评估了在几个时间点的血钠异常(血清钠<135或>145 mmol/L,低钠血症和高钠血症)与住院患者死亡率、需要高级通气支持和急性肾损伤(AKI)之间的相关性。
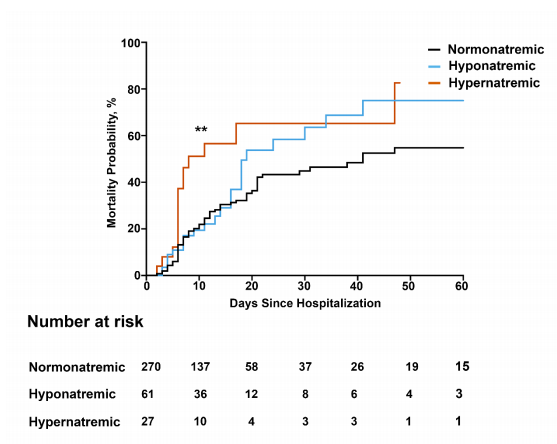
该研究纳入了488位患者(中位年龄为68岁)。在就诊时,24.6%的患者有低钠血症,主要是由于血容量不足,而5.3%的患者伴有高钠血症。与正常人相比,入院后两天内发生的高钠血症和住院期间任何时间点暴露于高钠血症,死亡风险分别增加2.34倍(95%CI为1.08-5.05,p=0.0014)和3.05倍(95%CI为1.69-5.49,p<0.0001)。入院时低钠血症与需要通气支持的可能性增加了2.18倍相关(95%CI为1.34-3.45,p=0.0011)。除低血容量性低钠血症亚组外,低钠血症不是院内死亡的危险因素。血钠水平与AKI风险和住院时间长短无关。
由此可见,住院期间血钠异常是COVID-19患者预后不良的危险因素,高钠血症和低钠血症分别与更大的死亡和呼吸衰竭风险相关。血钠水平可用于COVID-19患者的危险分层。
原始出处:
Ploutarchos Tzoulis.et al.Dysnatremia is a predictor for morbidity and mortality in hospitalized patients with COVID-19.JCEM.2021.https://doi.org/10.1210/clinem/dgab107
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血钠#
61
#JCE#
54
#JCEM#
53
#发病率#
59
#预测指标#
59