
乳腺癌治疗可影响患者躯干和上肢淋巴和肌肉骨骼系统,针对腋窝的手术和放疗后的不良后遗症很常见,多达三分之一的患者会经历肩关节活动受限、慢性疼痛和淋巴水肿,影响患者生活质量和恢复进程,特别是接受了腋窝清扫或腋窝/锁骨上放疗的患者,其发生肩关节和上肢相关残疾的风险增加。近日研究人员考察了运动对乳腺癌手术后上肢残疾高风险人群生活质量及运动能力的影响。

本次研究在英国17个国家卫生服务和癌症中心开展,382名乳腺癌手术患者参与,其术后上肢残疾风险高,随机接受结构化运动(n=191)或常规护理(n=191)。结构化运动组在常规护理基础上,接受物理治疗主导的运动计划,包括伸展、强化、体育活动和行为改变以实现长期坚持锻炼,在术后7-10天开始,在第1个月和3个月进行两次预约干预。研究的主要终点为12个月时手臂、手、肩(DASH)残疾问卷,次要结果包括DASH分量表、疼痛、并发症、与健康相关的生活质量和医疗资源使用。
参与者平均年龄58.1岁,运动组中,181人(95%)至少接受了1次干预。与对照组相比,运动后,患者上肢功能显著改善(运动组DASH得分为16.3 vs 对照组22.9,平均差异为7.81)。次要终点方面,运动组也更具优势:运动组12个月时疼痛强度较低(平均差异-0.68),手臂残疾症状较少(FACT-B+4:-2.02)。运动不会增加并发症、淋巴水肿或不良事件风险。与常规护理相比,运动组花费的医疗资源更少(平均减少387英镑)。
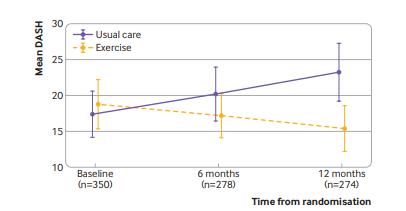
运动对患者上肢功能的改善作用
研究认为,建议乳腺癌术后患者积极接受结构化运动干预,可有效降低上肢残疾风险。
原始出处:
Julie Bruce et al. Exercise versus usual care after non-reconstructive breast cancer surgery (UK PROSPER): multicentre randomised controlled trial and economic evaluation.BMJ. 11 November, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BMJ#
76
很好
218
#乳腺癌患者#
68
谢谢分享
220
学习#乳腺癌#
236
不错
217
很有意思
218