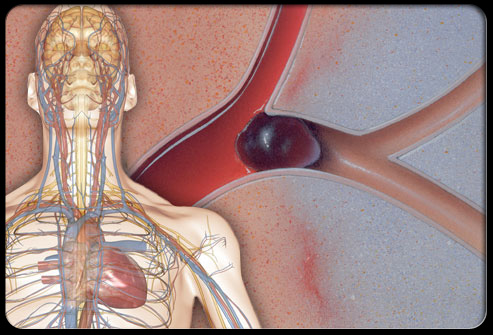
Cochrane DB Syst Rev:急性缺血性卒中后LMWHs抗血栓治疗的“是是非非”
2017-05-02 梁舒瑶 ;常路 环球医学
低分子量肝素(LMWHs)和肝素类似物是比标准普通肝素(UFH)具有更强抗血栓效果的抗凝剂,同时出血并发症风险也较低。2017年4月,发表在《Cochrane Database Syst Rev.》的一篇文章为这些药物的原始Cochrane回顾的更新,该回顾首次发表于2001年,末次更新于2008年。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#卒中后#
52
#缺血性#
45
#缺血性卒#
48
感谢分享,谢谢!
85
学习了,值得分享
88
#抗血栓治疗#
96
#抗血栓#
45
好内容,值得收集
77
学习了分享了
104
继续学习中谢谢
89