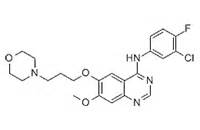
J CLIN ONCOL:吉非替尼在EGFR拷贝数增益的食管癌患者中疗效显著
2017-06-15 叶枫红 CPhI制药在线
食管癌吉非替尼(COG)试验是专门针对化疗耐药性食管癌二线治疗的唯一一个III期随机试验,包括食管腺癌和食管鳞癌。在COG试验中,450名患者被随机分配到吉非替尼组合安慰剂组。吉非替尼组患者的无进展生存期(PFS)和报告结果(PROs)均得到改善,反映出少数亚组患者对吉非替尼发生快速持久的反应。食管鳞癌和食管腺癌患者对吉非替尼的受益率相等。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
68
#食管癌患者#
71
#拷贝数#
81
文章很好,值得拜读
119
学习了谢谢分享!!!
101
#食管#
65
#GFR#
61
很不错的介绍
109