Cancers:结直肠癌(CRC)患者辅助化疗后血浆中CEA, CA19-9, IL-6, CRP,和 YKL-40水平预测疾病进展的提前时间和预后作用
2021-08-04 yd2015 MedSci原创
辅助化疗后升高的CEA, IL-6, 和CRP水平与较差的无病生存(DFS)有关,而IL-6和CRP水平与较差的总生存(OS)有关。预测疾病进展的提前时间中CEA最短。
结直肠癌(CRC)是常见的消化道恶性肿瘤之一。目前越来越多的研究探索结直肠癌中的预后指标。我们临床上常用的有CEA和CA199等。也有较多研究表明IL-6, CRP,和 YKL-40水平在结直肠癌中起到作用。但是这些指标在结直肠癌患者术后辅助化疗后预测疾病进展的提前时间和预后作用不明确。近期,有研究团队进行相关研究,结果发表在Cancers杂志上。
该研究纳入的是III期研究LIPSYT (ISRCTN98405441)中II–IV期结直肠癌(CRC)患者147例,其进行24周的5-FU为基础的辅助化疗。中位年龄60岁。88%为 II 或 III期。其中12例患者辅助治疗期间出现进展被排除,中位随访时间为11.9年 (range, 8.9–12.7)。5年和10年DFS率分别为54% 和50%, 5年和10年OS率分别为69% 和55%。
研究表明,辅助化疗后升高的CEA (HR=5.21, 95%CI 2.32–11.69), IL-6(HR=3.72, 95%CI 1.99–6.95), 和CRP (HR=2.58, 95%CI 1.18–5.61)水平与较差的无病生存(DFS)有关。
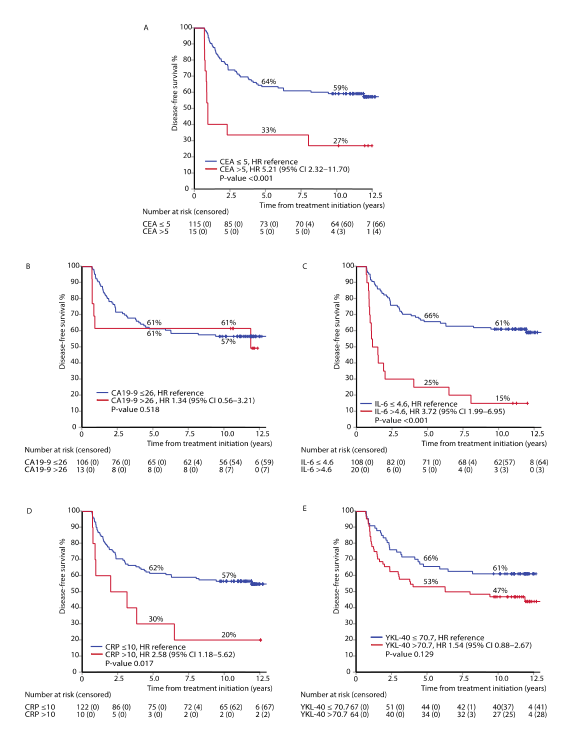
DFS
而辅助化疗后升高的IL-6 (HR=3.06, 95%CI 1.64–5.73)和CRP(HR=3.41, 95%CI 1.55–7.49)水平与较差的总生存(OS)有关。
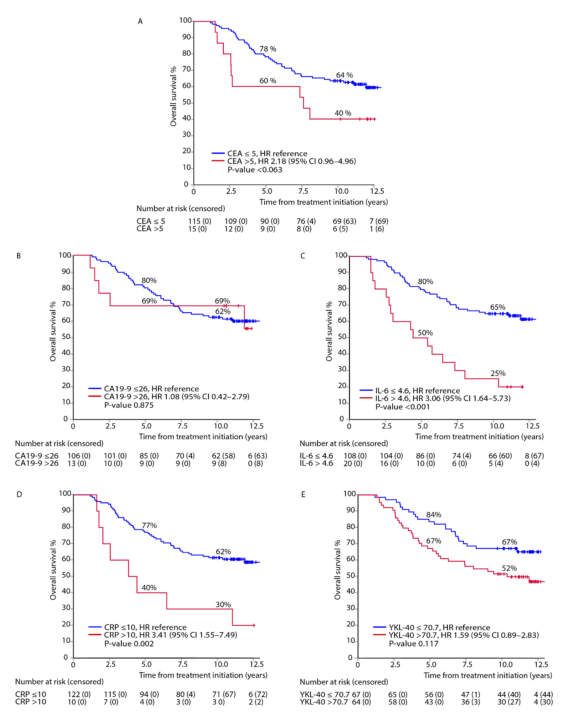
OS
进行校正的多因素分析发现,辅助化疗后升高的CEA 和IL-6跟较差的DFS相关, 而IL-6 and CRP跟较差的OS相关。
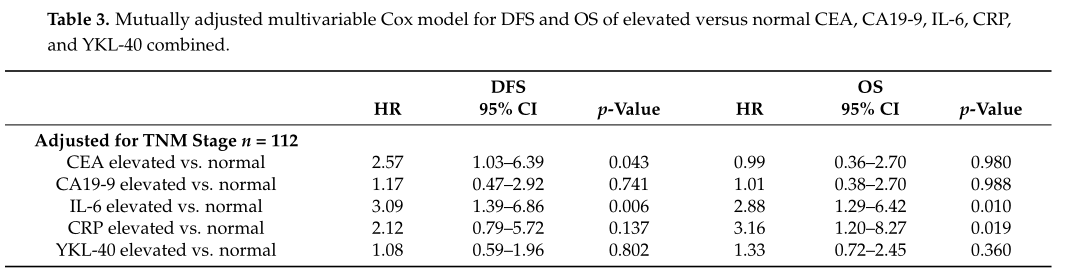
多因素DFS和OS相关因素分析
对于CEA正常(<5 µ g/L)的患者中,升高的IL-6 与较差的DFS(HR=3.12, 95%CI 1.38–7.04)和OS(HR=3.20, 95%CI 1.39–7.37)相关。而升高的CA19-9, CRP, 或YKL-40跟DFS和OS没有统计学差异。
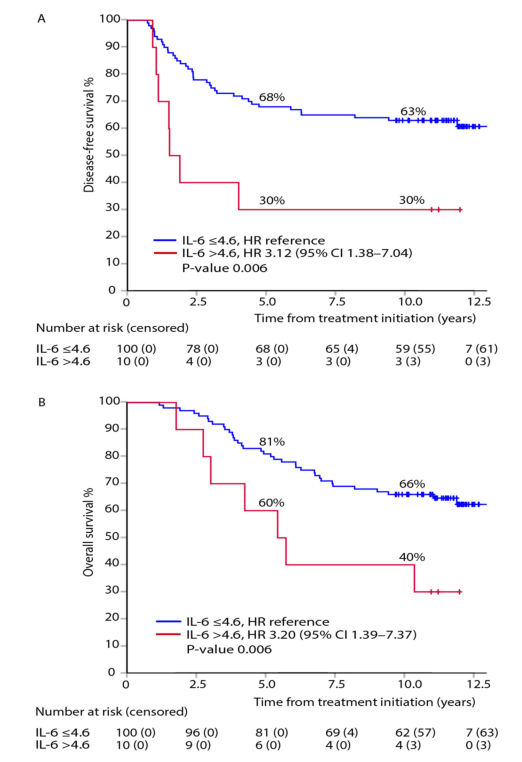
CEA正常IL-6升高DFS和OS比较
疾病进展的提前时间(Lead time)定义为第一次发现升高至影像学或临床诊断局部进展或远处转移的时间。CEA为7.8个月,CA199为10.0个月,IL-6为21.8个月,CRP为10.2个月,YKL-40为53.1个月。五个指标中任何一个出现升高时的提前时间为27.3个月。
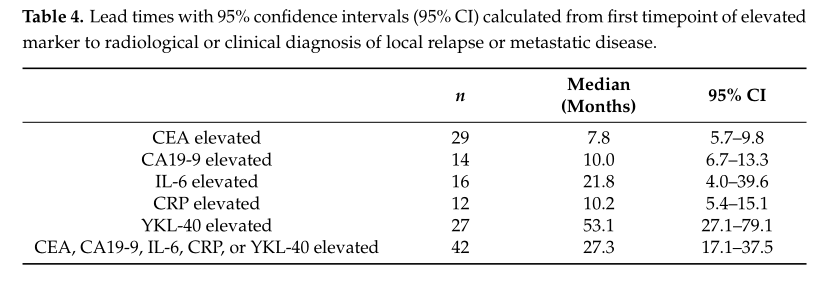
预测疾病进展的提前时间(Lead time)
综上,辅助化疗后升高的CEA, IL-6, 和CRP水平与较差的无病生存(DFS)有关,而IL-6和CRP水平与较差的总生存(OS)有关。预测疾病进展的提前时间中CEA最短。
原始出处:
Lehtomäki, K.; Mustonen,H.; Kellokumpu-Lehtinen, P.-L.; et al. Lead Time and Prognostic Role of Serum CEA, CA19-9, IL-6, CRP, and YKL-40 after Adjuvant Chemotherapy in Colorectal Cancer. Cancers 2021, 13, 3892. https://doi.org/10.3390/cancers13153892.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ERS#
63
#CRC#
62
#疾病进展#
63
#CRP#
0
#IL-6#
103
#结直肠#
59
#CEA#
68