盘点:近期白血病指南及重要研究汇总
2016-10-14 MedSci MedSci原创
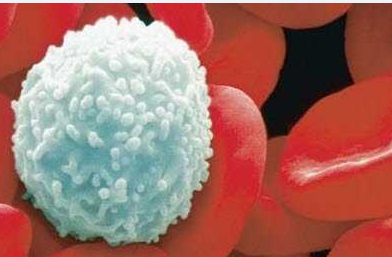
白血病是一类造血干细胞恶性克隆性疾病。克隆性白血病细胞因为增殖失控、分化障碍、凋亡受阻等机制在骨髓和其他造血组织中大量增殖累积,并浸润其他非造血组织和器官,同时抑制正常造血功能。临床可见不同程度的贫血、出血、感染发热以及肝、脾、淋巴结肿大和骨骼疼痛。这里梅斯小编整理了近期关于白血病指南共识及重要研究进展与大家分享。【1】2017 NCCN临床实践指南:慢性淋巴细胞白血病/小淋巴细胞淋巴瘤(20
白血病是一类造血干细胞恶性克隆性疾病。克隆性白血病细胞因为增殖失控、分化障碍、凋亡受阻等机制在骨髓和其他造血组织中大量增殖累积,并浸润其他非造血组织和器官,同时抑制正常造血功能。临床可见不同程度的贫血、出血、感染发热以及肝、脾、淋巴结肿大和骨骼疼痛。这里梅斯小编整理了近期关于白血病指南共识及重要研究进展与大家分享。
【1】2017 NCCN临床实践指南:慢性淋巴细胞白血病/小淋巴细胞淋巴瘤(2017.V1)
2016年9月,美国国家综合癌症网络(NCCN)发布了慢性淋巴细胞白血病/小淋巴细胞淋巴瘤指南2017年第一版,该指南的前一版来自2016年第3版非霍奇金淋巴瘤指南的部分。(文章详见——2017 NCCN临床实践指南:慢性淋巴细胞白血病/小淋巴细胞淋巴瘤(2017.V1))
【2】2015 NICE技术评估指南:Idelalisib治疗慢性淋巴细胞白血病(TA359)
2015年10月,英国国家卫生与临床优化研究所 (NICE)发布了Idelalisib治疗慢性淋巴细胞白血病的第359号技术评估指南。(文章详见——2015 NICE技术评估指南:Idelalisib治疗慢性淋巴细胞白血病(TA359))
【3】2015 ESMO恶性淋巴瘤共识会议建议:成熟的B细胞淋巴瘤和慢性淋巴细胞白血病的预测工具
2015年6月,欧洲肿瘤内科学会(ESMO)成熟的B细胞淋巴瘤和慢性淋巴细胞白血病共识会议在瑞士卢加诺召开,在会议上成熟的B细胞淋巴瘤和慢性淋巴细胞白血病的预测工具提出了相关建议,主要建议涉及:临时PET检查,TP53突变和缺失,通过IHC或 GEP测定COO以及基于分子的MRD评估为预测工具的潜在作用。(文章详见——2015 ESMO恶性淋巴瘤共识会议建议:成熟的B细胞淋巴瘤和慢性淋巴细胞白血病的预测工具)
【4】2016 NCCN临床实践指南:急性髓性白血病(2016.V2)
2016年6月,美国国家综合癌症网络(NCCN)发布了急性髓性白血病指南2016第2版,指南更新摘要如下:急性白血病和诊断研究评估(AML-1)
APL,诱导治疗(AML-2)
APL,巩固后治疗(AML-5)
APL,复发治疗(AML-7)
AML,治疗反应(年龄<60y)(AML-7)
AML,标准剂量阿糖胞苷诱导缓解后治疗(年龄<60y)(AML-8)
AML,大剂量阿糖胞苷诱导缓解后治疗(年龄<60y)(AML-9)
AML,缓解后治疗(年龄<60y)(AML-10)
AML,诱导治疗(年龄>60y)(AML-11)
AML,标准剂量阿糖胞苷诱导后治疗(年龄≥60y)(AML-12)
AML,缓解后治疗(年龄≥60y) (AML-13)
AML,监测(AML-14)
AML,复发/难治性疾病的治疗(AML-14)
基于验证细胞遗传学和分子异常风险状态(AML-A)
CNS淋巴瘤的评估和治疗(AML-B)
支持性治疗(AML-C)
急性髓系白血病反应标准(AML-D)
治疗期间监测(AML-E)
复发/难治性疾病的治疗(AML-F)(文章详见——2016 NCCN临床实践指南:急性髓性白血病(2016.V2))
【5】在年轻的急性髓系白血病(AML)患者中,多参数流式细胞术对微小残留病变(MRD)的预后研究
预处理预测基线时的急性髓系白血病(AML)患者的预测结果是其管理的基础。因此近些年来,治疗后的预后因素被评价得越来越多。
阿糖胞苷治疗中(总共≥5克/平方米)、甲氧基诱导化疗且达到缓解的280名年轻患者,以及对骨髓标本通过8-color多参数流式细胞仪检测的灵敏度为0.1%或更高的186名微小残留病变(MRD)患者被纳入了研究。
结果,诱导治疗至完全缓解(CR),166例患者需要1-2个月,79%MRD转为阴性,且MRD阴性状态与无复发生存率和总生存的改善相关。116例患者在巩固期达到MRD状态,86%MRD转为阴性,MRD阴性状态与RFS和OS显著相关。69例患者的MRD状态在所有的治疗完成后达到,84%MRD转为阴性,MRD阴性状态与RFS和OS的改善相关。多变量分析包括年龄、细胞遗传学反应和MRD后,发现MRD阴性状态是RFS和OS最重要的独立预测因素,在整个过程中,并在完成治疗时。
根据多参数流式细胞术,达到MRD阴性状态与接受阿糖胞苷+去甲氧基诱导的年轻AML患者高度显著改善的后果相关。(文章详见——Cancer:在年轻的急性髓系白血病(AML)患者中,多参数流式细胞术对微小残留病变(MRD)的预后研究)
【6】Cell新研究“歪打正着”发现白血病治疗新靶点
近日,来自美国麻省总医院和哈佛干细胞研究所的研究人员发现了一种治疗急性髓系白血病(AML)的新方法。在这篇发表在国际学术期刊Cell上的文章中,研究人员发现抑制一个特定代谢酶的作用能够促进白血病细胞的分化,减少它们的数目,降低它们形成癌症的能力。
在AML这种疾病中会发生许多基因的改变,该文章作者提出癌变过程中髓样干细胞分化的阻断需要经过几个重要的分子事件。研究人员在这些分子事件组成的通路上发现了一个潜在靶点,并且对于多数类型的AML来说这个靶点是共同的。在这项研究中,研究人员开发了一种筛选HoxA9抑制剂的新方法。
他们首先利用小鼠髓样细胞通过基因工程方法过表达HoxA9建立了一个AML的细胞模型,当细胞达到成熟状态就会发出绿色荧光。随后研究人员筛选了超过33万个小分子希望找到能够让细胞产生绿色信号的小分子,绿色信号的出现意味着HoxA9 诱导的分化阻断得到了疏通。最终只有12种化合物能够实现这一目标,研究人员发现其中有11种通过抑制一个叫做DHODH的代谢酶发挥作用,到目前为止还没有研究表明DHODH在髓样细胞分化过程中发挥作用。进一步实验表明抑制DHODH的活性确实能够诱导小鼠和人类AML细胞的分化。
研究人员随后在几种AML小鼠模型中检测了一种已知的DHODH抑制剂,发现了一套能够抑制白血病细胞的剂量方案,能够延长生存时间,同时不会出现常规化疗导致的副作用。研究人员发现6周的治疗不能阻止最终的复发,而10周的治疗似乎可以使疾病得到长期缓解,包括白血病干细胞的数目减少。他们在移植了人类AML细胞的小鼠模型上也观察到了类似的结果。
研究人员表示,如果抑制DHODH治疗AML的背后机制能够得到进一步研究,将为临床试验的开展提供更多依据。(文章详见——Cell新研究“歪打正着”发现白血病治疗新靶点)

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










好好学习
94
希望继续有突破
94
希望最终有实质性突破
95
了解下了
87
学习了,赞一个~
104
继续关注
57
好文章值得阅读
48