Circulation:细数主动脉瓣置换术相关影响因素
2015-09-30 张旭栋 MedSci原创
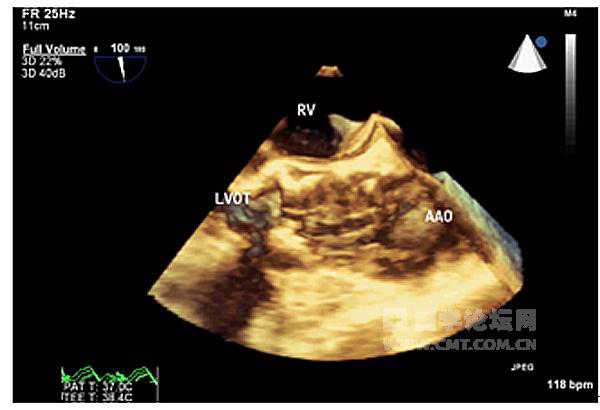
背景:依据术前左心室(LV)功能,明确主动脉瓣置换术(AVR)后,死亡率与充血性心力衰竭之间的关联;并描述发病率,手术时机,左心室恢复与左心室逆转之间的关联。方法和结果:研究纳入了3112例AVR术的患者,对后续临床超声心动图进行了为期中位6年的随访。手术时,他们的平均年龄为67.8±13.4年,其中三分之一为女性,29%左室功能不全(射血分数<50%)。严重主动脉狭窄和左心室功能不全的患者
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#置换#
75
#主动脉瓣#
57
#主动脉瓣置换术#
55
#主动脉#
49
#影响因素#
63
#置换术#
57