骨肉瘤是最常见的原发性骨恶性肿瘤,多发生于青少年或儿童。相比其他实体瘤,骨肉瘤的恶性程度高,预后较差,且由于骨肉瘤位置特殊,完全切除可能会对患者的肢体造成损伤,严重的可能导致截肢。因此,能够保证患者肢体健全的同时实现对肿瘤控制的放射疗法在骨肉瘤治疗领域起到了重要的作用。
质子重离子治疗作为世界先进的放疗手段,可以实现对骨肉瘤的精准放疗,在保证骨肉瘤治疗效果的同时,提高患者后续的生活质量。
质子重离子治疗骨肉瘤生存率高达75%
2021年,发表在权威医学期刊《RADIOTHERAPY AND ONCOLOGY(放射肿瘤学)》的研究证实,质子重离子可以显著提高骨肉瘤的预后效果,生存率可达75%!
▲图源:参考来源[1]
该研究纳入了2011年8月至2018年9月期间确诊的原发性、转移性或复发性,不能手术的骨肉瘤患者,并采用54 Gy 的质子治疗和18 Gy的重离子治疗。
结果显示,在患者治疗一年后,局部控制率(LPFS)为73%,无进展生存率(PFS)为60%,总生存率为75%;治疗两年后,局部控制率为55%,无进展生存率为45%,总生存率为68%;且研究人员并没有发现严重的毒副作用。
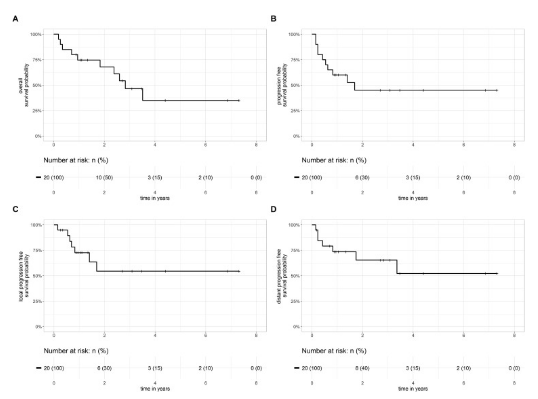
▲图源:参考来源[1]
质子重离子治疗骨肉瘤控制率达92%
2017年由日本研究人员开展的,发表在《Int J Radiat Oncol Biol Phys》的临床研究针对质子重离子治疗骨与软组织肿瘤的效果进行了汇总分析
该研究纳入了2005年5月至2014年12月确诊的91名骨与软组织肉瘤患者,包括脊索瘤、软骨肉瘤及骨肉瘤,其中82名患者是原发性,9名患者是复发性。所有患者都接受了70.4 Gy的质子或重离子治疗。
研究结果显示,质子重离子治疗骨与软组织肿瘤的3 年总生存率 (OS)、无进展生存率 (PFS) 和局部控制率分别为 83%、72% 和 92%;且患者并未出现任何毒副作用。
▲图源:参考来源[2]
骨与软组织肿瘤是骨肿瘤与软组织肿瘤的统称,包括骨肉瘤、尤文肉瘤、软骨肉瘤、脊索瘤等多种肿瘤。
除此之外,还有多项研究可以证实质子重离子治疗骨肉瘤的效果:
-
2011年发表在《Cancer》杂志中的研究显示,质子治疗骨肉瘤的3年和5年局部控制率(LC)分别为82%和72%,五年的无病生存率(DFS)为65%,总生存率(OS)为67%。
-
2015年重离子多中心临床研究(J-CROS)的数据显示,重离子治疗骨与软组织肿瘤的5年局部控制率为68%,5年生存率为65%。
参考来源:
[1]The role of combined ion-beam radiotherapy (CIBRT) with protons and carbon ions in a multimodal treatment strategy of inoperable osteosarcoma - Radiotherapy and Oncology
https://www.thegreenjournal.com/article/S0167-8140(21)06037-0/fulltext
[2] Demizu Y, Jin D, Sulaiman NS, Nagano F, Terashima K, Tokumaru S, Akagi T, Fujii O, Daimon T, Sasaki R, Fuwa N, Okimoto T. Particle Therapy Using Protons or Carbon Ions for Unresectable or Incompletely Resected Bone and Soft Tissue Sarcomas of the Pelvis. Int J Radiat Oncol Biol Phys. 2017 Jun 1;98(2):367-374. doi: 10.1016/j.ijrobp.2017.02.030. Epub 2017 Feb 22. PMID: 28463156.
[3] Proton-Based Radiotherapy for Unresectable or Incompletely Resected Osteosarcoma
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3716000/
[4] 骨軟部腫瘍に対する重粒子線治療について|今井礼子 - QST病院(旧放射線医学総合研究所病院)|重粒子線治療(がん治療)
https://www.nirs.qst.go.jp/hospital/radiotherapy/explanation/doctor08.php
- END -
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#重离子#
0
#患者预后#
79
#生存率#
120
#精准#
94
#质子重离子#
73
#精准放疗#
70