图文:气管插管教程
2015-05-08 MedSci 网络
一、指征 1、是否有气道保护失败? 2、是否有通气或氧合的失败? 3、预期的疾病发展(颈部血肿、全麻手术) 二、禁忌症 气管插管无绝对的禁忌症,气管不完全横断的患者视为相对禁忌。 三、用物的准备 手套、口罩、帽子、吸引器(插管前检查是否正常)、球囊面罩(连接好氧气源)、10ml 注射器、布胶带、气管导管(如果时间允许,检查气囊)、管芯、合适镜身的喉镜、听诊器。
一、指征
1、是否有气道保护失败?
2、是否有通气或氧合的失败?
3、预期的疾病发展(颈部血肿、全麻手术)
二、禁忌症
气管插管无绝对的禁忌症,气管不完全横断的患者视为相对禁忌。
三、用物的准备
手套、口罩、帽子、吸引器(插管前检查是否正常)、球囊面罩(连接好氧气源)、10ml 注射器、布胶带、气管导管(如果时间允许,检查气囊)、管芯、合适镜身的喉镜、听诊器。
四、病人的准备
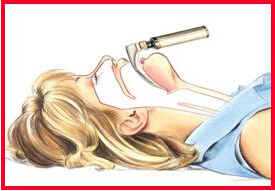
预吸氧,使患者的血氧饱和度竟可能的提高,但患者饱和度不能迅速提高时应该果断进行插管;镇静药物使用;体位(平卧位,头、颈、身体保持一直线;修正体位:头枕部垫一小方枕,使头抬高10cm);心电监护;静脉通道;知情同意书
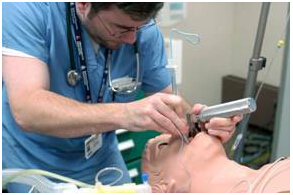
五、操作过程
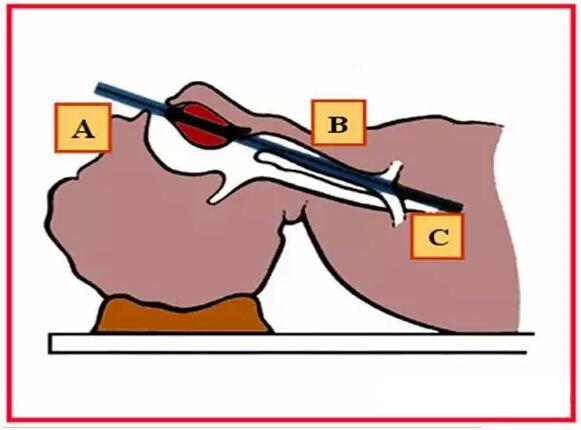
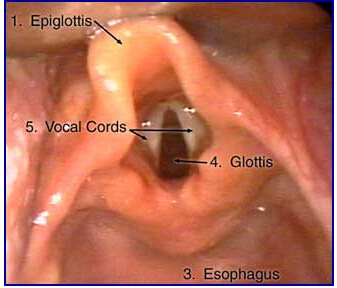
1、插管:左手握住喉镜,右手使患者口腔张开。把喉镜镜身插入病人右舌方。逐渐移动镜身到口中央,把舌压到左侧。缓慢插入镜身定位到会厌。如果用的是弯型,则要把它放到会厌谷,即舌跟和会厌之间,喉镜向前上提45 度角,就可以看到声带。沿着喉镜手轴向病人足侧方向推进。手腕不要弯,摇动镜片防止病人牙齿的咬合,这时候要避免牙齿和软组织损伤。右手握气管导管,从病人右侧口角插入气管导管。插管不应把声带视野阻挡,这是操作的关键部分。插管通过声带进入气管直到球囊消失,抽出针芯,空气膨胀球囊到防止漏气所要最小压力,一般要求5-10ml 的空气。
2、确认导管位置:五点听诊法(胃、双上肺、双下肺);呼吸末二氧化碳探测器;胸部x线检查;胸廓起伏;导管水雾;血氧饱和度上升。
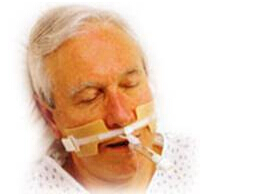
3、固定导管:布胶带固定;固定器固定。



六、气管插管的并发症:插入食道;误吸;局部损伤出血;心律血压影响。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












刚好要考试 很有帮助
73
不错学习并收藏!
128
暴露对我是个问题
120
赞
168
还行
133
图文并茂,不错
113
感兴趣
147
#气管插管#
63
好东东
120
看看
101