BMC Cancer:徐兵河院士团队分析中国汉族人群转移性乳腺癌伴有同时性肺转移患者的临床病理特征和生存预后
2021-12-28 yd2015 MedSci原创
该研究提供了中国汉族人群首次诊断MBC时伴有肺转移(BCLM)患者的临床病理特征和生存结果的重要信息。
肺转移是乳腺癌第二常见的远处转移部位,临床上约占转移性乳腺癌(MBC)患者的15-25%。包括化疗、靶向治疗和内分泌治疗在内的系统治疗被推荐用于乳腺癌肺转移(BCLM)的患者,肺转移切除术对于适当选择的病例也是推荐的。早期发现肺转移,准确判断预后,有利于乳腺癌患者在临床实践中获得长期生存。然而,在汉族人群中,BCLM的临床病理特征和影响发病率和预后的危险因素仍有待明确。因此,中国医学科学院肿瘤医院徐兵河院士团队开展了相关研究,分析中国汉族人群转移性乳腺癌伴有同时性肺转移(BCLM)患者的临床病理特征和预后。相关结果发表在BMC Cancer杂志上。
研究筛查2000年4月至2019年9月间首次诊断的3155例MBC患者的临床资料,最终纳入MBC患者2263例,其中809例患者首次诊断MBC时出现肺转移。采用多因素logistic回归分析确定BCLM的危险因素,采用单因素和多因素Cox回归分析评估BCLM患者的预后因素。
2263例MBC患者中,同时性肺转移(BCLM)患者有809例(35.7%)。BCLM患者中HR+/HER2-、HR- /HER2+、HR+/HER2+和三阴性亚型分别占47.7、14.3、16.1和21.9%。与其他亚群相比,三阴性亚型肺转移患者更年轻(p = 0.015),原发乳腺癌N分期更早(p = 0.005), DFS更短(p<0.001),复发性疾病较多(p = 0.002),肝转移较少(p = 0.001)。HER2+ (HR /HER2+和HR+/HER2+) BCLM患者比HER2- (HR+/HER2-和三阴性)患者更容易诊断为新发IV期乳腺癌(p = 0.002)。BCLM患者中HR+/HER2-亚型骨转移瘤发生率最高(p <0.001)。
2263例MBC中,HR+/HER2-、HR- /HER2+、HR+/HER2+和三阴性亚型分别占52.1, 13.3, 16.1和18.5%。肺转移的发生率分别为32.7,38.6,35.6和42.3%。总体肺转移率为35.7%。
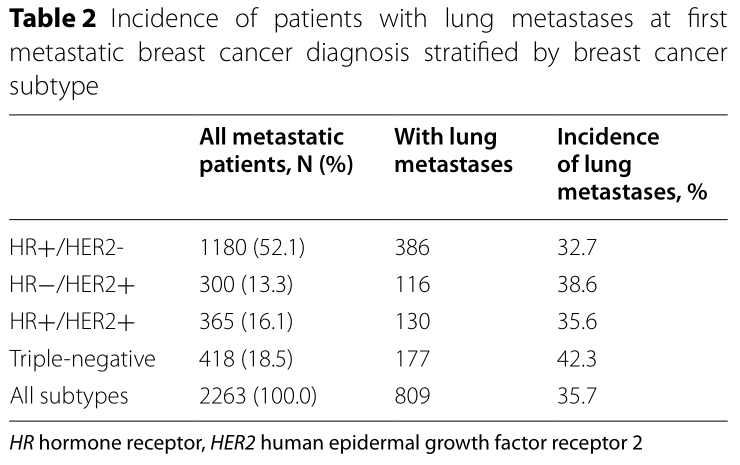
不同乳腺癌亚型肺转移发病率
年龄≥50岁(vs <50岁,OR = 1.29,95% CI 1.54 = 1.08, p = 0.005), ECOG=2(vs ECOG 0,OR= 1.67,95% CI 2.67 = 1.04, p = 0.033), M1(vs M0,OR= 1.42,95% CI 1.92 = 1.05, p = 0.022),HR-/ HER2 +亚型(vs HR+ / HER2 -, OR= 1.40, 95% CI 1.85 = 1.06, p = 0.020),三阴性亚型(vs HR+ / HER2 -, OR= 1.63, 95% CI 2.09 = 1.28, p<0.001)和DFS>2年(vs. DFS<2年,OR = 1.74, 95% CI = 1.42 2.14, p<0.001)与诊断时肺转移的发病率增高显著相关。侵袭性小叶癌(ILC) (vs 侵袭性导管癌(IDC),OR = 0.39, 95% CI = 0.22 0.70, p = 0.002)和骨转移(vs.无骨转移,OR = 0.74, 95% CI = 0.61 0.90, p = 0.002)与诊断时肺转移的发病率低显著相关。
整个MBC队列患者中位随访时间为61.6个月,中位生存期为45.4个月。MBC伴有肺转移患者的中位OS明显较无肺转移患者差,分别为41.7个月和47.9个月(p=0.001)。
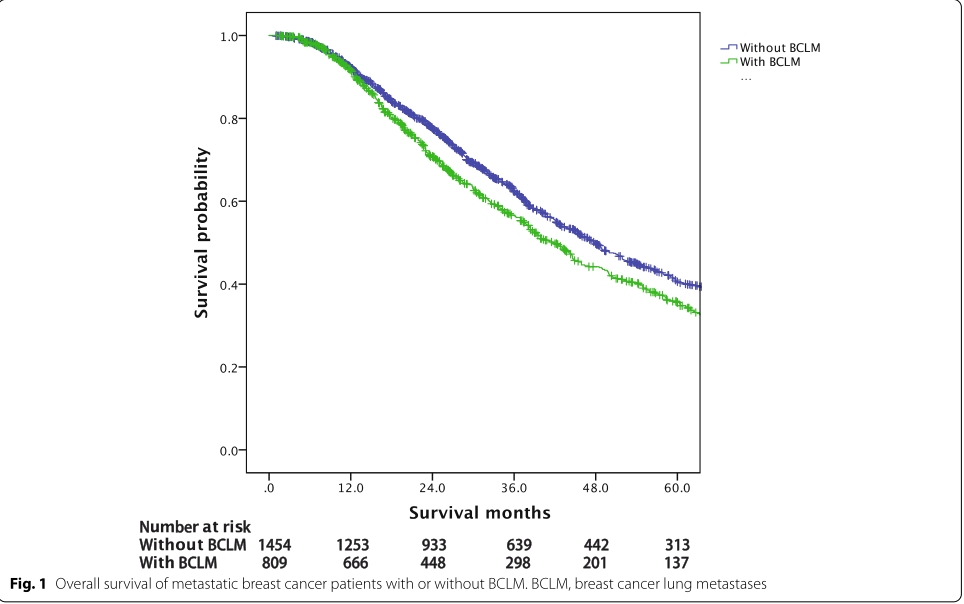
MBC有无肺转移的预后差异
HR+/HER2-亚型BCLM患者的生存期最长(49.0个月),而三阴性(26.8个月,p<0.001)最短。HR- /HER2+ (vs. HR+/HER2-, p = 0.009)和HR+/HER2 + (vs. HR+/HER2-,p = 0.746)亚型BCLM患者的中位OS分别为31.6个月和44.1个月。
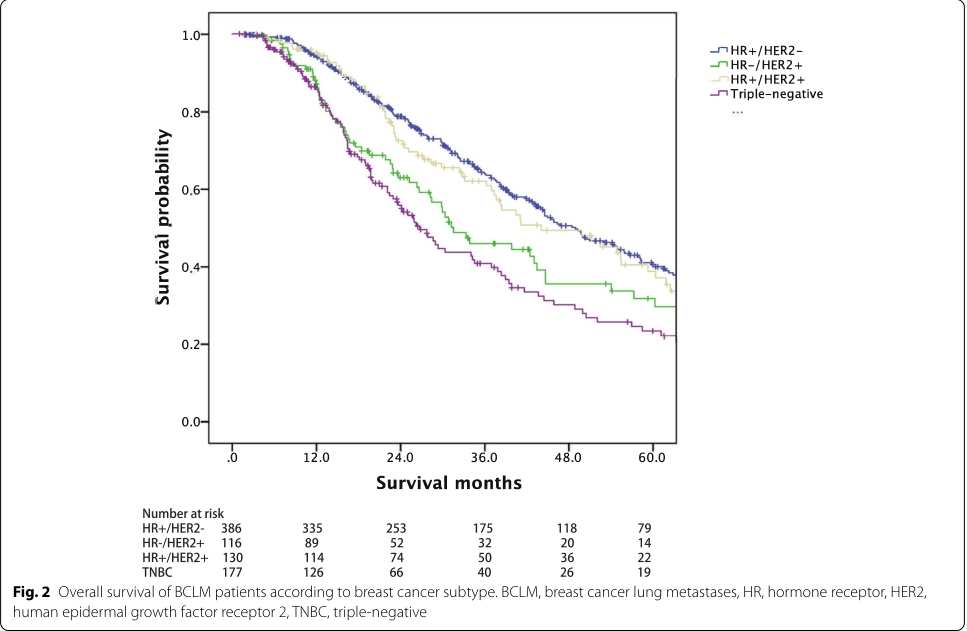
BCLM患者不同分子亚型的预后差异
三阴性亚型(vs. HR+/HER2-,HR = 1.76, 95% CI = 1.36 2.29, p<0.001)、肝转移(vs.无肝转移,HR = 2.19, 95% CI = 1.70 2.82, p<0.001), 2个转移部位(vs. 1个转移部位,HR = 1.76, 95% CI = 1.34 2.31, p<0.001)、≥3个转移部位(vs. 1个转移部位,HR = 1.74, 95% CI = 1.24 2.44, p = 0.001)与BCLM患者的较差生存期显著相关。DFS>2年(vs. DFS≤2年,HR = 0.66, 95% CI = 0.53 0.83, p<0.001)与BCLM患者良好预后相关。
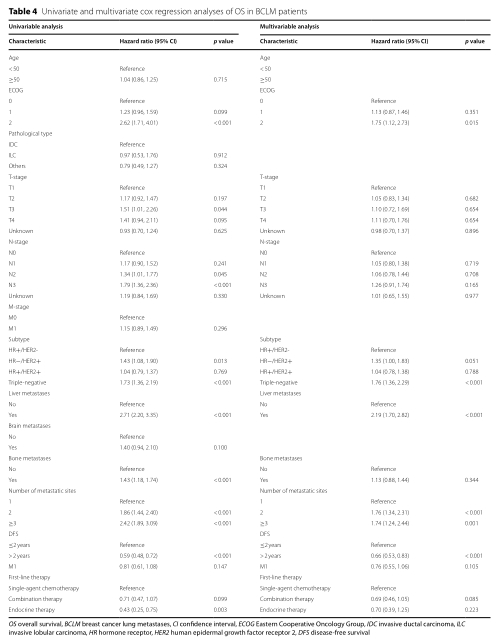
BCLM患者OS多因素分析
综上,该研究提供了中国汉族人群首次诊断MBC时伴有肺转移(BCLM)患者的临床病理特征和生存结果的重要信息。
原始出处:
Lin S, Mo H, Li Y, Guan X, Chen Y, Wang Z, Xu B. Clinicopathological characteristics and survival outcomes in patients with synchronous lung metastases upon initial metastatic breast cancer diagnosis in Han population. BMC Cancer. 2021 Dec 14;21(1):1330. doi: 10.1186/s12885-021-09038-2. PMID: 34906122; PMCID: PMC8670055.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#徐兵河#
86
#BMC#
56
#汉族人群#
64
#病理特征#
86
#临床病理#
102
#生存预后#
139
厉害,学习了
81
#转移性#
71
#肺转移#
92