BMJ:这个患者为啥呼吸困难和腹部肿胀-案例报道
2017-02-16 xing.T MedSci原创
Meigs综合征是由良性纤维瘤引起胸腔积液和腹水,而假Meigs综合征是原发或继发卵巢恶性肿瘤引起的。
患者为一名50岁的女性,在数周内出现呼吸急促伴腹胀和不适而就诊。她无法平躺,由于端坐呼吸。该患者没有其他疾病以及药物治疗。进行了胸部、腹部和盆腔计算机断层扫描(CT)扫描,其次是活检和诊断性手术治疗。术后组织学证实为良性肿瘤。该患者CT图像有哪三个主要的影像学发现(如图1所示),这个经典的三联征相关同名诊断是啥?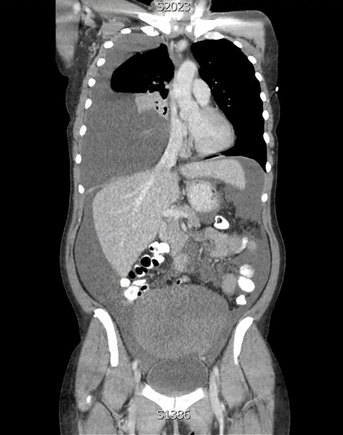
图1胸部、腹部和骨盆的冠状计算机断层扫描(CT)图像
答案
CT显示右侧大量胸腔积液,导致纵隔移位和严重腹水(如图2所示)。有一个来自于骨盆的大肿块。良性卵巢纤维瘤相关的胸腔积液或腹水被称为Meigs综合征。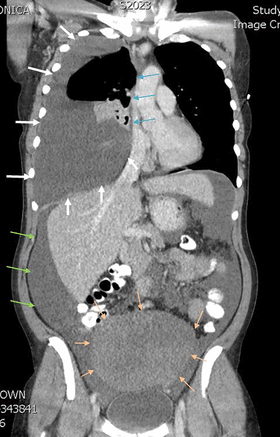
图2大量的右侧胸腔积液(白色箭头)引起纵隔移位(蓝箭头)。有一个来自于骨盆的大肿块(橙色箭头),这增加了恶性肿瘤或纤维瘤的可能性。也存在大量腹水(绿色箭头)
患者预后
该患者接受经腹全子宫及双侧卵巢切除手术切除了纤维瘤后,恢复良好,腹水和胸腔积液得以解决。
学习要点
Meigs综合征是由良性纤维瘤引起胸腔积液和腹水,而假Meigs综合征是原发或继发卵巢恶性肿瘤引起的。
快速转诊接受进一步调查和诊断是必需的。腹水或胸水引流可以缓解症状,但最终根治的方法是纤维瘤切除。
原始出处:
Jennifer Kahan,et al. Breathlessness and abdominal swelling: a classic eponymous syndrome.BMJ 2017; 356 doi: https://doi.org/10.1136/bmj.j382
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#BMJ#
39
#呼吸困难#
48
好好努力
65