Blood:IL-7R信号——预防T-ALL复发的重要靶点!
2019-09-18 MedSci MedSci原创
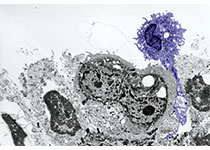
急性T淋巴细胞白血病(T-ALL)是一种侵袭性恶性血液病,由调控胸腺T细胞发育的信号通路失调引起。复发率高,复发患者的预后极其不良。因此,开发新的特异性靶向调控白血病启动细胞(LIC)活性的通路的新疗法对治疗难治性T-ALL至关重要。白细胞介素-7受体(IL-7R)是T-ALL中普遍表达的一条重要的T细胞发育通路,与白血病的进展密切相关。但IL-7R/IL-7信号在T-ALL病理过程中的作用以及对
急性T淋巴细胞白血病(T-ALL)是一种侵袭性恶性血液病,由调控胸腺T细胞发育的信号通路失调引起。复发率高,复发患者的预后极其不良。因此,开发新的特异性靶向调控白血病启动细胞(LIC)活性的通路的新疗法对治疗难治性T-ALL至关重要。
白细胞介素-7受体(IL-7R)是T-ALL中普遍表达的一条重要的T细胞发育通路,与白血病的进展密切相关。但IL-7R/IL-7信号在T-ALL病理过程中的作用以及对该疾病复发的贡献尚未明确。为了直接探索IL-7R靶向治疗T-ALL复发是否有效,研究人员采用一种明确的NOTCH1诱导的T-ALL模型,因为大多数T-ALL患者都存在NOTCH1突变激活的情况,而NOTCH1是IL-7R表达的转录调控因子。
采用功能丧失性方法,研究人员发现用Il7r缺陷小鼠组成性激活Notch1的造血前体细胞移植到免疫缺陷小鼠上时,不能诱发白血病,而野生型小鼠的可诱发,证明了IL-7R的功能对于Notch1诱导的T细胞白血病发生必不可少。此外,研究人员还证明了IL-7R表达是具有LIC潜能的T-ALL细胞的早期功能性生物标志物,并证实IL-7R信号受损会阻碍患者来源的T-ALL移植瘤的定植和进展。值得注意的是,研究人员还发现IL-7R依赖性的LIC活性和白血病进展可以扩展到人类的B-ALL。
综上所述,本研究具有重要的治疗意义,强调了靶向IL-7R信号或可用于治疗干预,特别是预防T-ALL(和B-ALL)复发。
原始出处:
Sara González-García, et al.IL-7R is essential for leukemia-initiating cell activity and pathogenesis of T-cell acute lymphoblastic leukemia.Blood 2019 :blood.2019000982; doi: https://doi.org/10.1182/blood.2019000982
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#IL-7R#
74
#ALL#
78
#T-ALL#
70