Nature Biotechnology:高血压延迟病毒清除并加剧COVID-19患者的气道炎症
2021-01-12 MedSci原创 MedSci原创
合并高血压的COVID-19患者更有可能发生严重并发症,这也使他们面临更大的死亡风险。科学家现在发现,高血压患者的免疫细胞已经被预先激活,而且这种预先激活在COVID-19下大大增强。
在COVID-19住院患者中,男性和老年患者发生危重疾病的风险较高。高血压在全球成年人中非常普遍,已被确定为COVID-19严重程度增加的主要危险因素。伴有COVID-19的高血压患者比无高血压的患者更有可能发展为严重肺炎或器官损害。此外,这些患者表现出加重的炎症反应,比无高血压的患者死于COVID-19的风险更高。
据推测,通过ACEIs或ARBs的抗高血压治疗可能会调节ACE2的表达,从而改变SARS-CoV-2感染的易感性。在经典的RAAS通路中,血管紧张素II与血管紧张素II受体亚型1 (AT1R)结合,促进血管收缩和促炎症反应。另一方面,ACE2将血管紧张素II裂解为血管紧张素1-7和血管紧张素I裂解为血管紧张素1-9,两者都具有血管扩张和抗炎作用。
动物研究数据表明,ACEIs和ARB可上调ACE2表达,这就产生了一个问题:在接受ACEIs或ARB治疗的患者中,SARS-CoV-2受体的增加是否使他们更容易受到病毒感染和传播。迄今为止,没有来自观察性研究的证据表明ACEI或ARB治疗可增加SARS-CoV-2的传染性。
高血压与炎症过程的激活有关。由于呼吸系统中的一种高炎症表型被描述为增强了COVID-19的严重性。近日,发表在Nature Biotechnology上的一篇名为Hypertension delays viral clearance and exacerbates airway hyperinflammation in patients with COVID-19的研究评估了SARS-CoV-2感染前高血压患者潜在的促炎症倾向是否可能导致疾病严重性的加重。
Irina Lehmann实验室的研究小组组长Saskia博士报告说:“我们分析了32名COVID-19患者和16名未感染对照组的鼻咽共114761个细胞,两组都包括心血管病患者以及没有心血管问题的人。发现心血管病患者的免疫细胞甚至在感染新型冠状病毒之前就表现出强烈的预激活。在接触病毒后,这些患者更有可能产生增强的免疫反应,这与COVID-19的严重疾病进展有关。然而,我们的研究结果也表明,尽管不使用血管紧张素受体阻滞剂,但使用ACE抑制剂治疗可以防止冠状病毒感染后这种增强的免疫反应。因此,ACE抑制剂可以降低高血压患者经历严重疾病进展的风险。”
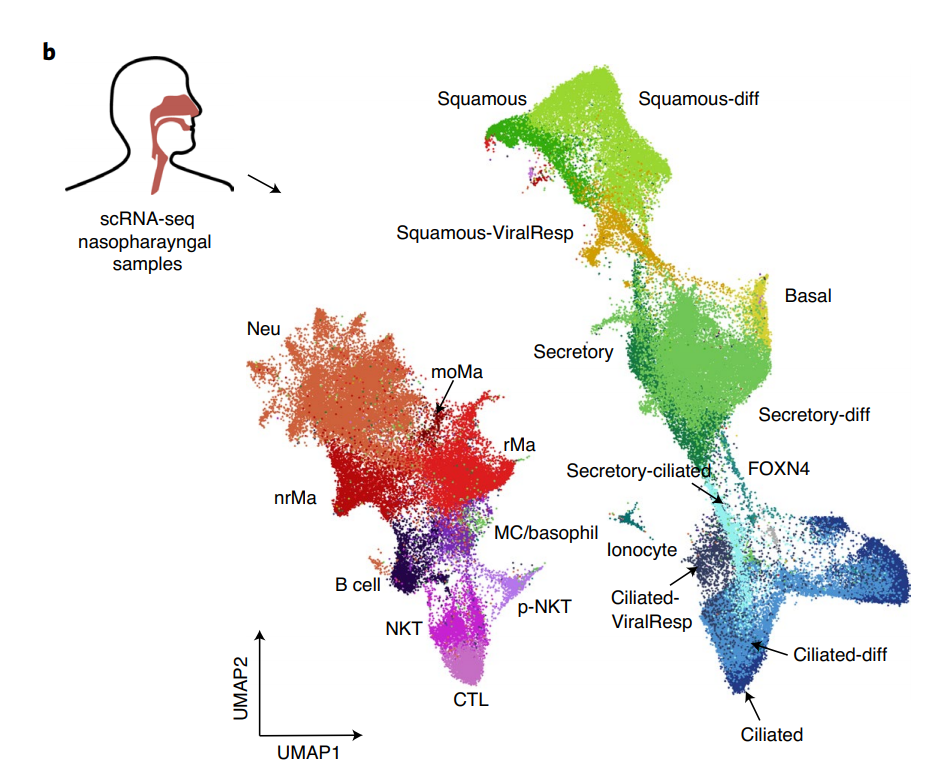
从患者的鼻咽部收集样本并进行scRNA-seq,使给定的UMAP显示所有识别的细胞类型和状态(颜色编码)。
此外,科学家们还发现,降压药还可以影响免疫系统降低病毒载量(即体内病毒浓度)的速度。波黑数字健康中心主任Roland Eils说:“在这里,我们观察到不同形式的高血压治疗有明显的不同。在接受血管紧张素II受体阻滞剂治疗的患者中,病毒载量的下降显著延迟,这也可能导致COVID-19病程更严重。在接受ACE抑制剂治疗高血压的患者中,我们没有观察到这种延迟。”
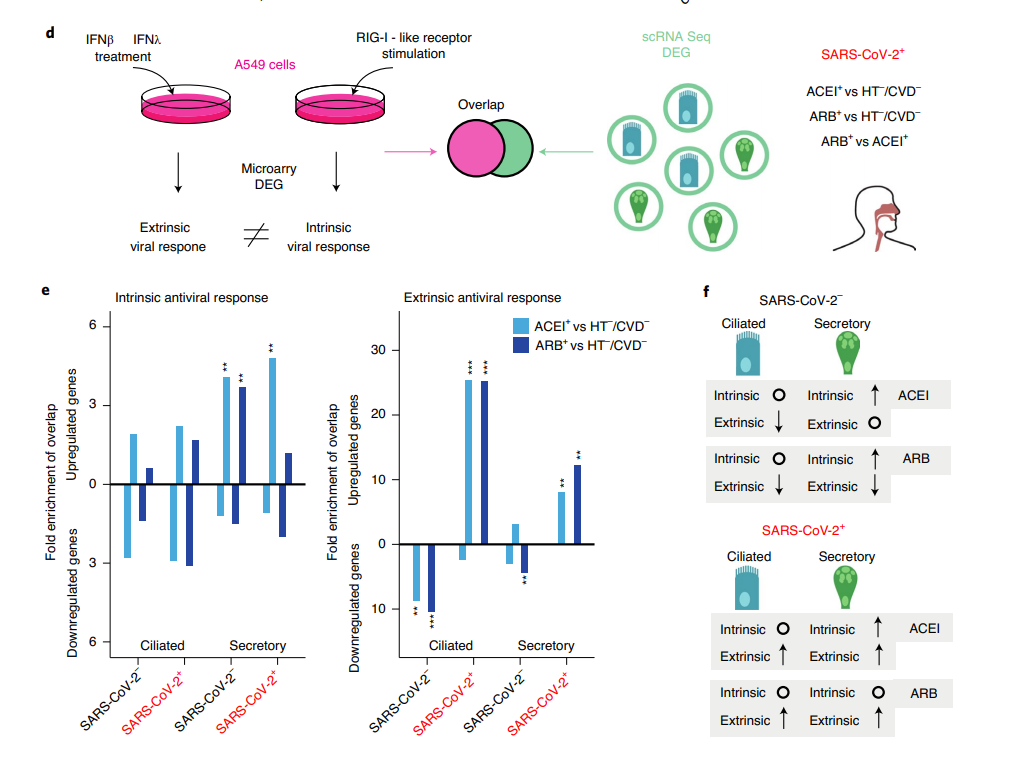
不同抗高血压治疗的患者抗病毒反应的差异调节。
40多名科学家一直在以极快的速度进行这项广泛的研究。Roland Eils解释说:“要想在大流行期间迅速对紧急问题提供答案,需要许多有献身精神的个人进行跨学科合作。COVID-19是一种非常复杂的疾病,我们召集了来自心脏病学、免疫学、病毒学、肺医学、重症监护和计算机科学的专家来进行这项研究。我们的目标是尽快就ACE抑制剂或血管紧张素受体阻阻剂同时治疗在COVID-19大流行期间是否会产生有利甚至不利影响这个问题提供科学合理的答案。”
总之,在本研究中,结合144例临床数据(n= 144)、48例气道样本的单细胞测序数据和体外实验,研究者观察到与COVID-19重症进展相关的高血压患者存在明显的免疫细胞炎症易感性。ACEI治疗与抑制COVID -19相关的过度炎症和增加细胞内在抗病毒反应有关,而ARB治疗与增强上皮免疫细胞相互作用有关。高血压患者的巨噬细胞和中性粒细胞,特别是在ARB治疗下,表现出更高的促炎细胞因子CCL3和CCL4以及趋化因子受体CCR1的表达。尽管我们的队列规模有限,无法确定临床疗效,但我们的数据表明,对于患有COVID-19的患者来说,使用血管紧张素转换酶抑制剂治疗高血压可能比使用血管紧张素II受体阻阻剂更有益——目前正在通过随机试验进一步研究这一假设。ACEI治疗患有高血压的COVID-19患者的临床益处值得进一步研究。
参考文献:Trump S, Lukassen S, Anker MS, Chua RL, Liebig J, Thürmann L, Corman VM, Binder M, Loske J, Klasa C, Krieger T, Hennig BP, Messingschlager M, Pott F, Kazmierski J, Twardziok S, Albrecht JP, Eils J, Hadzibegovic S, Lena A, Heidecker B, Bürgel T, Steinfeldt J, Goffinet C, Kurth F, Witzenrath M, Völker MT, Müller SD, Liebert UG, Ishaque N, Kaderali L, Sander LE, Drosten C, Laudi S, Eils R, Conrad C, Landmesser U, Lehmann I. Hypertension delays viral clearance and exacerbates airway hyperinflammation in patients with COVID-19. Nat Biotechnol. 2020 Dec 24. doi: 10.1038/s41587-020-00796-1. Epub ahead of print. PMID: 33361824.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
83
#Bio#
81
#TEC#
85
#Biotech#
124
#Technology#
79
#COVID-19患者#
78
#气道炎症#
90
很有意思的文献
125
非常好的分享
120
👍
123