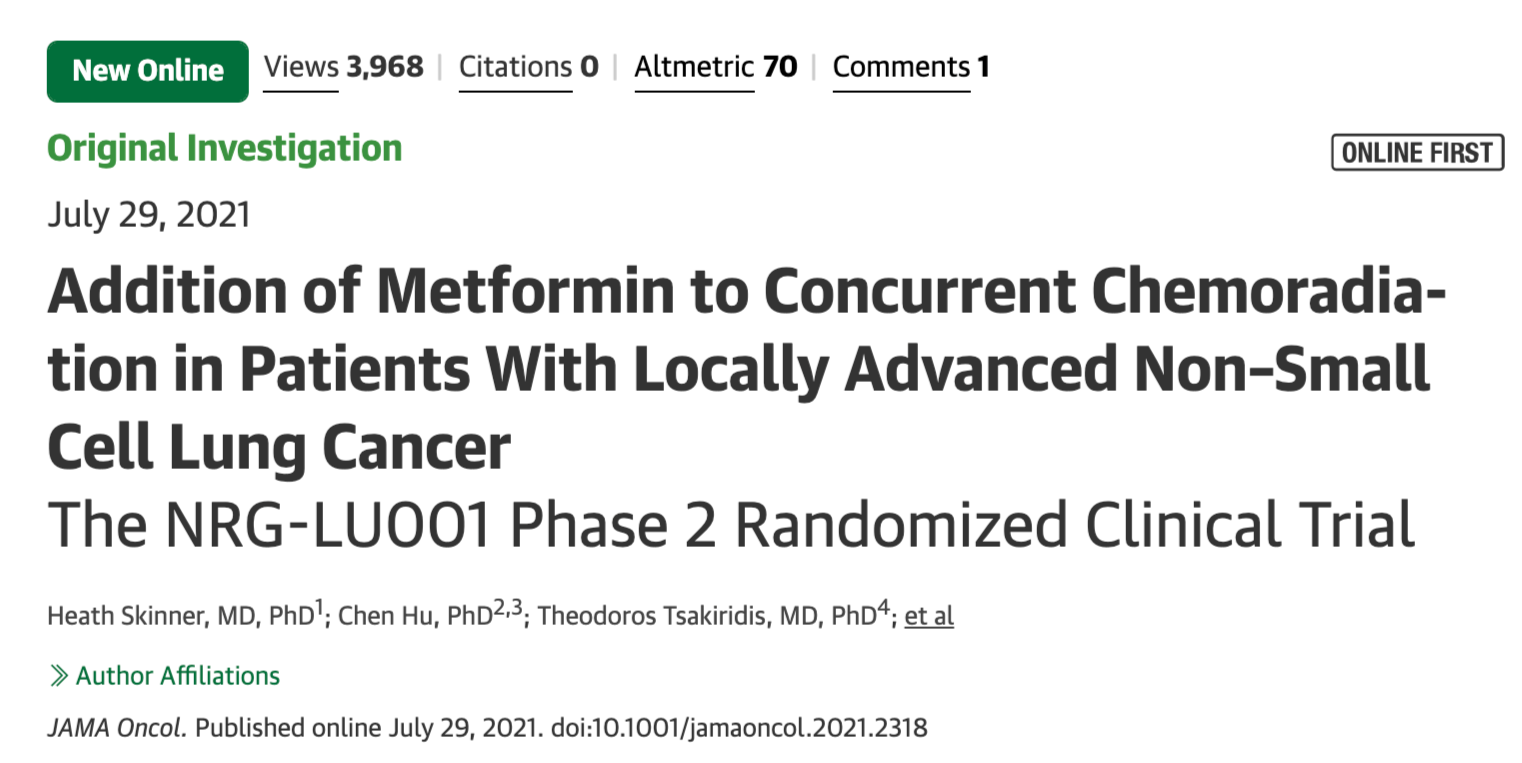
JAMA Oncol:二甲双胍联合同步放化疗治疗局部晚期非小细胞肺癌(NRG-LU001研究,附点评)
2021-08-12 MedSci原创 MedSci原创
二甲双胍作为神药,近年来相关研究很多,例如:“神药”二甲双胍,又发现34个新作用;其中二甲双胍预防肿瘤的发生,证据比较明确。但是,近年来出现许多有关二甲双胍辅助治疗肿瘤也相当多
二甲双胍作为神药,近年来相关研究很多,例如:“神药”二甲双胍,又发现34个新作用;其中二甲双胍预防肿瘤的发生,证据比较明确。但是,近年来出现许多有关二甲双胍辅助治疗肿瘤也相当多,毕竟预防与治疗是完全不同。二甲双胍能否治疗或辅助治疗肿瘤,仍然存在疑问。例如,Brit J Cancer:胃腺癌患者服用二甲双胍可改善预后;Brit J Cancer:二甲双胍与肺癌患者生存率的关系;Brit J Cancer:二甲双胍联合伊立替康治疗难治性大肠癌疗效分析;DCR:二甲双胍作为放射增敏剂在直肠癌新辅助治疗中的作用; 其机制一般认为与肿瘤微环境相关,见:Clin Cancer Res :二甲双胍杀伤肿瘤细胞之前先改造“土壤”;Clin Cancer Res:小剂量二甲双胍对食管癌肿瘤免疫微环境的影响; 因此,本研究是研究者针对Ⅲ期非小细胞肺癌时,比较单纯放化疗与单纯放化疗和二甲双胍治疗的疗效。研究结果发表在近日的JAMA oncology杂志上。 这项2期NRG-LU001随机临床试验是一项开放标签的2期研究,于2014年8月24日至2016年12月15日进行。无糖尿病且诊断为不可切除的III期非
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
71
#局部晚期#
131
#非小细胞#
109
#放化疗#
60
#局部#
61
#同步放化疗#
67
学习
92
赞同
81
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
94
谢谢梅斯分享这么多精彩信息
104