Radiother Oncol:功能影像学改变能预测晚期头颈部肿瘤患者对诱导化疗反应
2013-05-06 echo1166 互联网
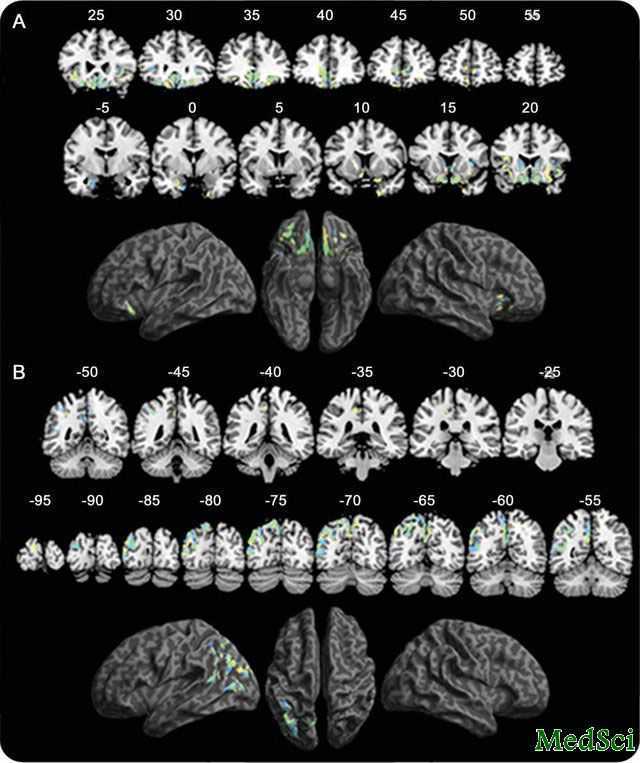
在头颈部肿瘤患者进行放化疗前首先进行诱导化疗时,功能影像能反映患者对最优治疗计划的适应性。因此,理解诱导化疗对功能影像的影响是必要的。为了前瞻性的评估获得序列 FI(18F-FDG-PET, 弥散加权(DW)和动态对比增强(DCE) MRI)的可行性以及其在确定头颈部肿瘤患者诱导化疗后个体治疗方案中的作用。为了解答上述问题,Ceri Powell等进行了相关研究,研究结果发表在Radiother
在头颈部肿瘤患者进行放化疗前首先进行诱导化疗时,功能影像能反映患者对最优治疗计划的适应性。因此,理解诱导化疗对功能影像的影响是必要的。为了前瞻性的评估获得序列 FI(18F-FDG-PET, 弥散加权(DW)和动态对比增强(DCE) MRI)的可行性以及其在确定头颈部肿瘤患者诱导化疗后个体治疗方案中的作用。为了解答上述问题,Ceri Powell等进行了相关研究,研究结果发表在Radiother Oncol 10月的期刊上。
10名III期和IV期的头颈部肿瘤患者被纳入研究,他们接受常规影像学检查和功能性影像学检查,前者包括CT和MRI,后者包括DW、DCE-MRI和18F-FDG-PET/CT。评估时间为入组时和进行了2个周期的诱导化疗后、确定放化疗方案之前。
有一名患者因为幽闭恐惧症从研究中脱落。18F-FDG-PET影像显示9名患者中有7人对诱导化疗出现完全代谢应答。DCE-MRI显示传输常数显着降低以及在60s时钆曲线下面积,DW-MRI显示诱导化疗后ADC增高。
在头颈部肿瘤患者进行功能性影像学检查是可行的。在进行诱导化疗后出现显着的功能影像学参数的变化能指导帮助制定个体化的治疗方案

10.1016/j.radonc.2012.09.009
PMC:
PMID:
Changes in functional imaging parameters following induction chemotherapy have important implications for individualised patient-based treatment regimens for advanced head and neck cancer
Ceri Powella, Maria Schmidta, Marco Borria, Dow-Mu Koha, Mike Partridgea, Angela Riddella, Gary Cookd, Shreerang A. Bhidea, c, Christopher M. Nuttingb, Kevin J. Harringtonb, c, Katie L. Newbolda
Background When induction chemotherapy (IC) is used prior to chemoradiotherapy (CRT) in head and neck cancer (HNC), functional imaging (FI) may inform adaptation of treatment plans with the aim of optimising outcomes. Understanding the impact of IC on FI parameters is, therefore, essential. Purpose To prospectively evaluate the feasibility of acquiring serial FI (18F-FDG-PET, diffusion-weighted (DW) and dynamic contrast-enhanced (DCE) MRI) and its role in defining individualised treatment regimens following IC in HNC. Methods and materials Ten patients with stage III and IV HNC underwent conventional (CT and MRI) and functional (DW, DCE-MRI and 18F-FDG-PET/CT) imaging at baseline and following two cycles of IC prior to definitive CRT. Results One patient withdrew due to claustrophobia. Seven out of nine patients had a complete metabolic response to IC on 18F-FDG-PET imaging. DCE-MRI showed a significant fall in transfer constant (Ktrans) (0.209 vs 0.129 min−1P < 0.01) and integrated area under gadolinium curve at 60 s (IAUGC6O) (18.4 vs 11.9 mmol/min, P < 0.01) and DW-MRI a rise in ADC (0.89 vs 1.06 × 10−3 mm2/s, P < 0.01) following IC. Conclusions Acquiring FI sequences is feasible in HNC. There are marked changes in FI parameters following IC which may guide adaptation of individualised treatment regimens.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Radiother#
70
#Oncol#
47
#化疗反应#
87
#肿瘤患者#
64
#头颈部#
58
#诱导化疗#
48
#颈部#
56