Photodiagnosis Photodyn Ther:维生素D3皮内注射与局部光动力疗法都可有效治疗顽固性掌跖疣
2021-08-25 MedSci原创 MedSci原创
顽固性掌跖疣的治疗十分困难,局部破坏性方法的副作用使得人们需要采用其他发病率较低的方式。最近,免疫以及激光疗法已成为新的治疗方法。近日,发表于的一项前瞻性、随机、对照的比较研究对比了皮内注射维生素D3
顽固性掌跖疣的治疗十分困难,局部破坏性方法的副作用使得人们需要采用其他发病率较低的方式。最近,免疫以及激光疗法已成为新的治疗方法。近日,发表于的一项前瞻性、随机、对照的比较研究对比了皮内注射维生素D3和使用曙红的光动力疗法(PDT)在治疗顽固性掌跖疣方面的安全性和疗效。
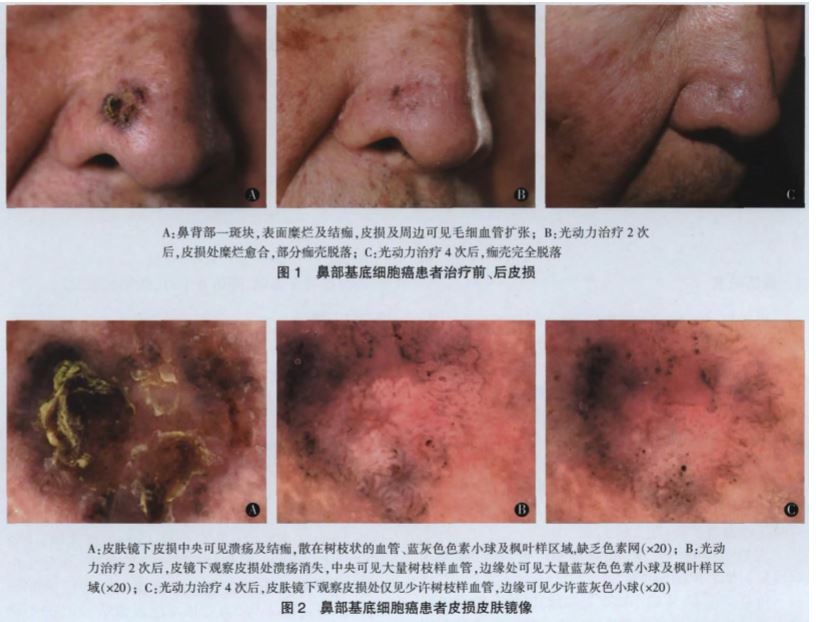
研究共纳入56名顽固性掌跖疣患者,随机分为3组:A组注射皮内维生素D3;B组接受PDT治疗,曙红作为光敏剂;C组为对照组。通过照片记录和皮肤镜评估,在基线、每个疗程前和完成治疗后,对临床改善进行评估。治愈后对患者进行了6个月的随访,以检测复发情况。
结果显示,A组和B组分别有88.89%和86.36%的患者完全治愈,而对照组有18.75%(P值<0.001)。除了A组在注射过程中出现疼痛外,没有其他副作用的报告。

综上所述,该研究结果表明,在目前的研究中,维生素D3和PDT疗法在治疗病毒性疣方面都是一种安全、高效和耐受性好的方式。
原始出处:
Nahla A Ibrahim, et al., Intralesional vitamin D3 versus new topical photodynamic therapy in recalcitrant palmoplanter warts Randomized comparative controlled study. Photodiagnosis Photodyn Ther. 2020 Dec;32:101979. doi: 10.1016/j.pdpdt.2020.101979.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#DIA#
101
#diagnosis#
73
#photo#
97
#顽固性#
75
#局部#
99
#光动力#
0
#有效治疗#
95
学习了
147