Nat. Cell Biol.:杨慕华研究组发现头颈癌扩散抑制因子
2012-04-10 台湾阳明大学 台湾阳明大学
杨慕华研究团队,左起:临医所博士生杨文豪、杨慕华与研究助理蓝欣怡 台湾阳明大学临床医学研究所杨慕及所领导的研究团队,在头颈癌临床医学研究上有重大的突破,他们发现头颈癌局部侵犯的关键“Twist1”蛋白,并发现抑制“RAC1”蛋白可作为头颈癌治疗的新标的。相关研究成果3月11日在线发表于《Nature Cell Biology》。 头颈癌包括口腔癌及咽喉癌,近年来在台湾发生率快速上升,成为国人男

杨慕华研究团队,左起:临医所博士生杨文豪、杨慕华与研究助理蓝欣怡
台湾阳明大学临床医学研究所杨慕及所领导的研究团队,在头颈癌临床医学研究上有重大的突破,他们发现头颈癌局部侵犯的关键“Twist1”蛋白,并发现抑制“RAC1”蛋白可作为头颈癌治疗的新标的。相关研究成果3月11日在线发表于《Nature Cell Biology》。
头颈癌包括口腔癌及咽喉癌,近年来在台湾发生率快速上升,成为国人男性癌症第四大死因。许多头颈癌病患是到晚期有明显症状时才发现。晚期头颈癌的特征为肿瘤在局部快速生长,造成头颈组织压迫、破坏与功能丧失。因头颈口咽部位为吞咽与构音相关的重要器官,晚期头颈癌常造成吞咽与发声困难,并引起外观上的巨大变化,对病患生理及心理都造成极大威胁。另外,对于晚期头颈癌,手术、化疗以及放射治疗的效果均不彰,是临床医师们最为棘手的病况。
杨慕华与研究团队成员(包括临医所博士生杨文豪与研究助理蓝欣怡),结合对头颈癌长期的临床观察与细胞生物学实验,发现头颈癌之所以具有局部高侵袭性的特殊临床表徵,是因癌细胞内转录因子Twist1藉由抑制微型RNA let-7i表现,引发RAC1活化,使头颈癌细胞在三维细胞培养系统中产生“间质型运动模式”。Twist1引发之“间质型运动模式”与头颈癌之局部侵犯性有高度相关,而使用RAC1抑制剂可阻断Twist1引发之间质运动。团队也在临床头颈癌组织印证上述发现:癌组织中若是同时有Twist1大量表现,以及let-7i表现减低之情况,病患肿瘤局部侵犯的情形最为严重。
杨慕华表示,这项研究具有科学上与临床上双重价值:在科学上,他们发现了头颈癌特有的局部侵袭性的分子机转,而临床上,他们提供了RAC1做为头颈癌新的治疗标的。因头颈癌为国人好发疾病,在欧美相对发生率较低,分子机转的研究相对也较少,这项研究对于发展头颈癌的个人化医疗,以及头颈癌专一标靶药物研发,将有重大助益。 (生物谷 bioon.com)

doi:10.1038/ncb2455
PMC:
PMID:
RAC1 activation mediates Twist1-induced cancer cell migration
Wen-Hao Yang,Hsin-Yi Lan,Chi-Hung Huang,Shyh-Kuan Tai,Cheng-Hwai Tzeng,Shou-Yen Kao,Kou-Juey Wu,Mien-Chie Hung& Muh-Hwa Yang
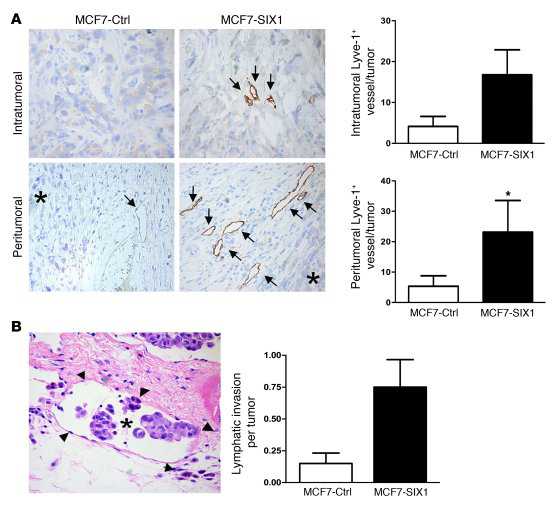
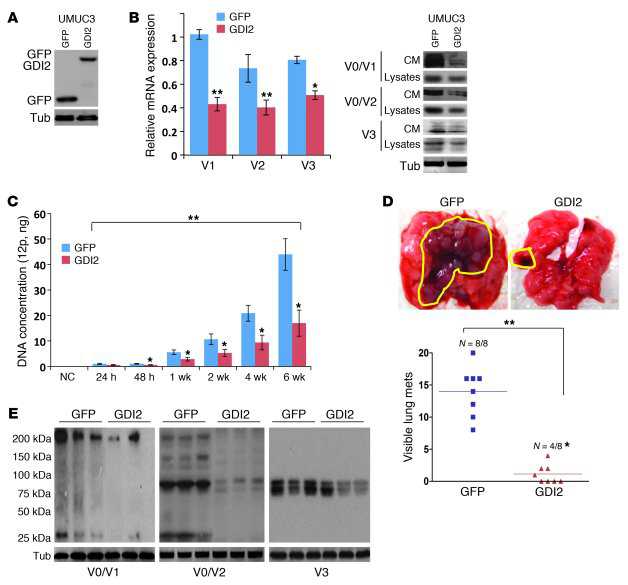
Epithelial–mesenchymal transition (EMT), which is characterized by the suppression of the adhesion protein E-cadherin, is a crucial process that promotes metastasis and stem-like properties of cancer cells. However, the dissociation of cellular aggregates is not sufficient to explain why cancer cells move, and the motile nature of cancer cells undergoing EMT remains elusive. Here, we identify a mechanism in which the EMT inducer Twist1 elicits cancer cell movement through activation of RAC1. Twist1 cooperates with BMI1 to suppress let-7i expression, which results in upregulation of NEDD9 and DOCK3, leading to RAC1 activation and enabling mesenchymal-mode movement in three-dimensional environments. Moreover, the suppression of let-7i contributes to Twist1-induced stem-like properties. Clinically, activation of the Twist1–let-7i–NEDD9 axis in head and neck cancer patients correlates with tumour invasiveness and worse outcome. Our results uncover an essential mechanism to explain how Twist1 induces the motile stem-like cancer cell phenotype beyond simply suppressing E-cadherin.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
45
#Bio#
62
#Biol#
57
#Nat#
51
#Cell#
48
#头颈癌#
53
#抑制因子#
56