JAHA:破裂和无症状完整的腹主动脉瘤患者峰值壁应力和峰值壁破裂指数比较
2021-04-15 MedSci原创 MedSci原创
与主动脉最大直径类似的无症状完整AAA相比,AAA破裂患者PWRI更大,而PWS则不然。
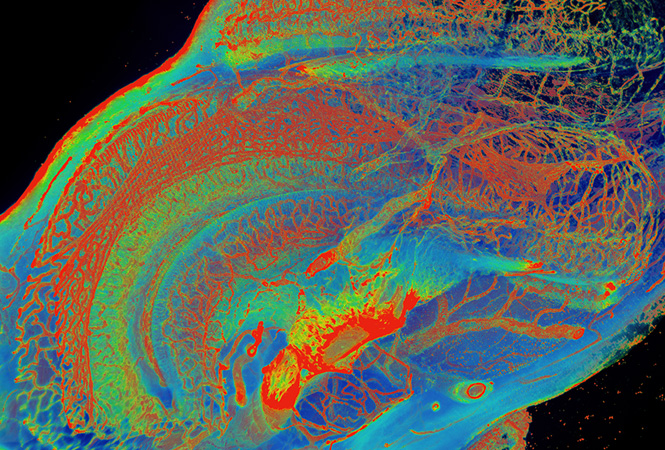
先前的研究表明,主动脉峰值壁应力(PWS)和峰值壁破裂指数(PWRI)可以估计腹主动脉瘤(AAA)的破裂风险,但是尚不清楚这些指标是否具有单独评估AAA直径的独立预测能力。
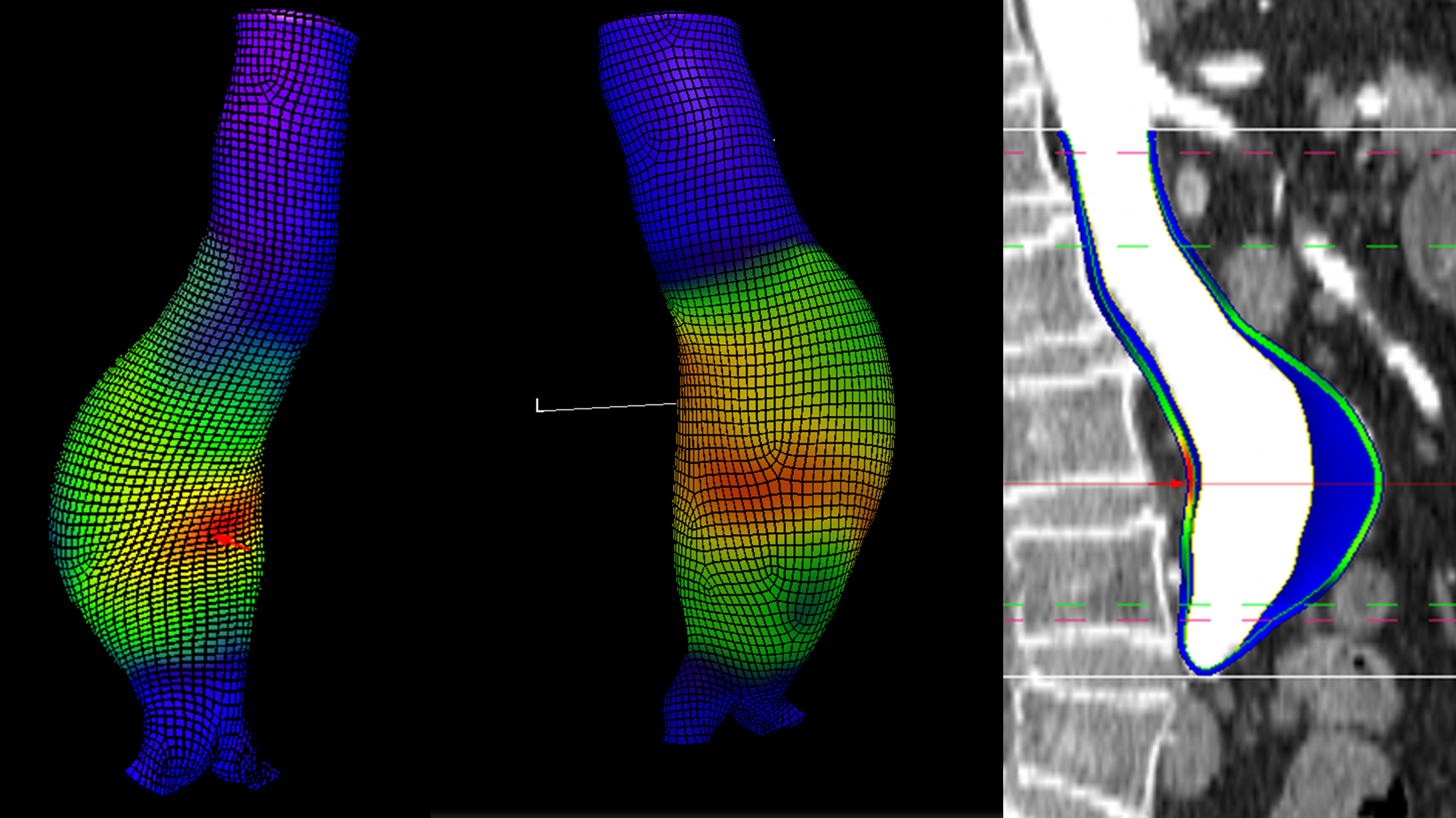
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该系统评价旨在比较具有相似直径的破裂和无症状完整AAA参与者PWS和PWRI的预测效能。

研究人员系统地检索了Web of Science、Scopus、Medline和Cochrane数据库,以确定评估PWS和PWRI在直径相似的破裂和无症状完整AAA中预测效能的研究。研究人员使用逆方差加权方法进行随机效应荟萃分析,并进行了敏感性分析,以评估结果的稳健性。研究人员通过改良的纽卡斯尔-渥太华量表和标准质量评估标准来评估偏倚风险,以评估主要的研究文献。
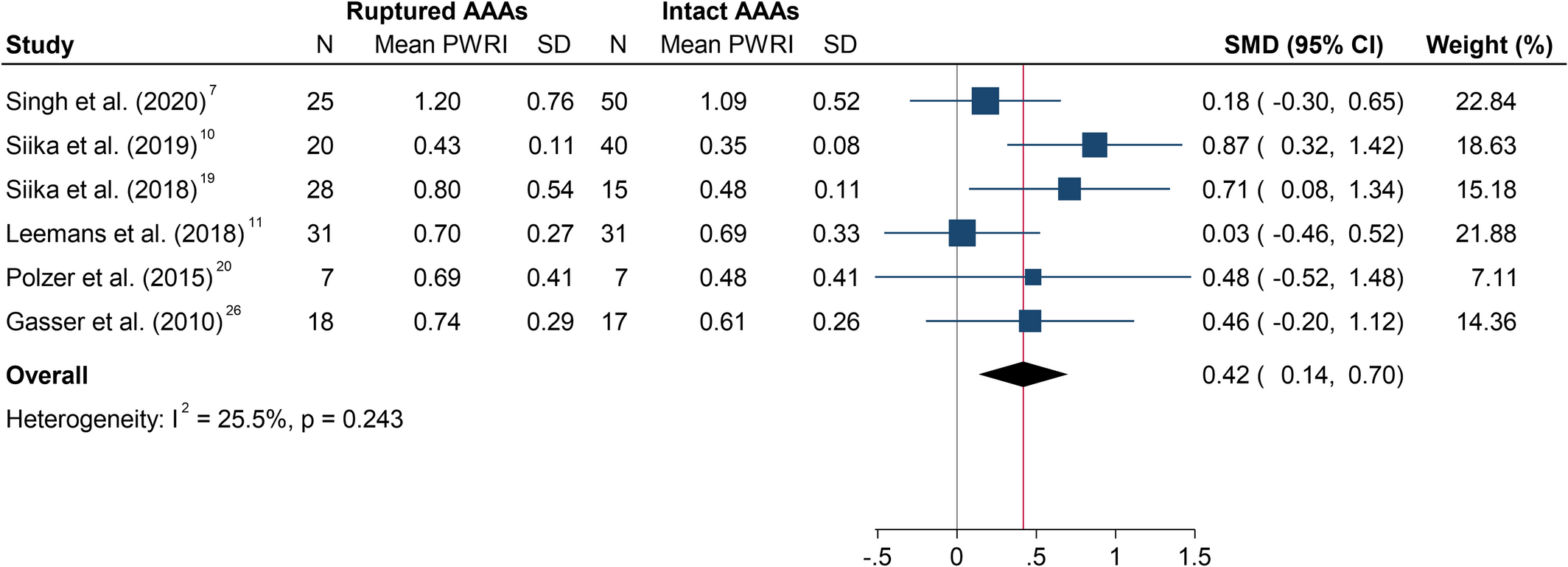
该分析纳入了包含309名参与者的七项病例对照研究。荟萃分析表明,相比于AAA完整患者,AAA破裂患者PWRI(标准化平均差异为0.42;95%CI为0.14-0.70;P=0.004)更大,而PWS(标准化平均差异为0.13;95%CI为-0.18至0.44;P=0.418)则不然。敏感性分析表明,研究结果不依赖于任何一项研究。纳入的研究被评估为具有中度到高度偏倚的风险。
由此可见,基于有限的证据,该分析表明,与主动脉最大直径类似的无症状完整AAA相比,AAA破裂患者PWRI更大,而PWS则不然。
原始出处:
Tejas P. Singh.et al.Systematic Review and Meta‐Analysis of Peak Wall Stress and Peak Wall Rupture Index in Ruptured and Asymptomatic Intact Abdominal Aortic Aneurysms.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.019772
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AHA#
46
#主动脉#
61
#主动脉瘤#
52
#无症状#
66
#应力#
69
学习了。
82