Cancer Cell:还在质疑高剂量维C抗癌?人体安全试验已通过
2017-04-02 佚名 转化医学网
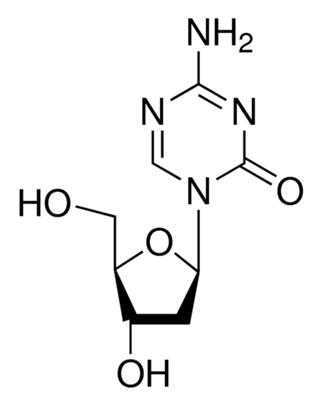
临床试验发现,定期给脑癌和肺癌患者注射800-1000倍日常服用量的维生素C作为改进常规癌症治疗效果的策略是安全的。在2017年3月30日提交的癌细胞研究工作报告中,爱荷华大学的研究人员展示了一令人惊讶的研究成果:改变癌细胞的铁代谢途径,导致癌细胞对高剂量维生素C引起的死亡敏感性增加。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













感谢分享
46
#CEL#
50
#质疑#
69
#Cell#
63
#高剂量#
0
#高剂量维C#
56
#cancer cell#
62
学习了,多谢分享
93