Rheumatology (Oxford):类风湿关节炎患者QTc延长影响预后
2014-03-11 佚名 MedSci原创
既往研究显示,类风湿关节炎(RA)患者心脏性猝死的几率较正常人高。而在长QT综合征的患者中,心律失常和心脏性猝死均与延长的QT间期相关。先天性QTc(校正后的QT间期)延长的患者出现心脏性猝死的死亡率高达13%。QTc是2型糖尿病患者死亡率的预测指标,而在2型糖尿病患者,其动脉粥样硬化性心血管疾病受累情况几乎与类风湿关节炎患者一致。【原文下载】 因此,探讨在高炎状态下的RA患者电生理(QT间期)
既往研究显示,类风湿关节炎(RA)患者心脏性猝死的几率较正常人高。而在长QT综合征的患者中,心律失常和心脏性猝死均与延长的QT间期相关。先天性QTc(校正后的QT间期)延长的患者出现心脏性猝死的死亡率高达13%。QTc是2型糖尿病患者死亡率的预测指标,而在2型糖尿病患者,其动脉粥样硬化性心血管疾病受累情况几乎与类风湿关节炎患者一致。【原文下载】
因此,探讨在高炎状态下的RA患者电生理(QT间期)对预测RA死亡率的作用尤为必要。来自英国伦敦汉姆史密斯医院的Vasileios F. Panoulas等人随访观察了具有详细的临床资料以及12导联心电图信息的357个RA患者,随访时间为73个月。运用线性回归和Cox回归对QTc的变量进行统计,并分析其与RA死亡率的相关性。
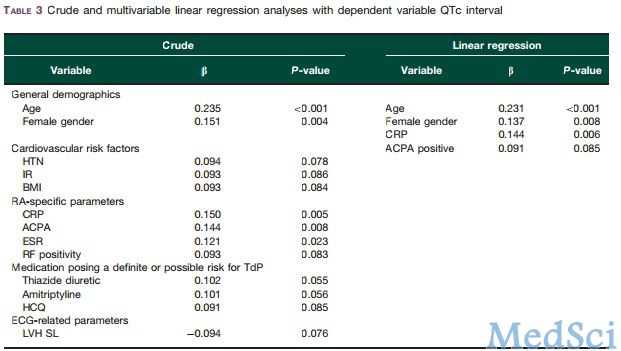
入组的患者平均年龄60.6岁,其中女性267位。共有54位RA患者(15.1%)在随访过程中死亡。年龄(P<0.001)、性别(P=0.008)和C反应蛋白(CRP)(P=0.006)均与QTc独立相关。QTc增加50毫秒死亡率危险比(HR)升高为2.17。按照心血管疾病(冠心病病史、高血压、胰岛素抵抗、吸烟史)和类风湿关节炎(HAQ评分、DAS评分、服用强的松)相关参数进行校正后,QTc与RA死亡率仍具有显著相关性。但把CRP纳入模型后分析则无统计学差异。
本研究发现,延长的QTc间期与RA患者死亡率相关。QTc与CRP的相关性也提示炎症与心律失常之间有潜在的相互作用。心电图是一种经济便利易行的临床检查,常规开展心电图检查明确QTc间期可以更好的提示类风湿关节炎患者预后,指导临床治疗。
原始出处:
Panoulas VF1, Toms TE, Douglas KM, Sandoo A, Metsios GS, Stavropoulos-Kalinoglou A, Kitas GD.Prolonged QTc interval predicts all-cause mortality in patients with rheumatoid arthritis: an association driven by high inflammatory burden.Rheumatology (Oxford). 2014 Jan;53(1):131-7. doi: 10.1093/rheumatology/ket338. Epub 2013 Oct 3.【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oxford#
56
#类风湿关节炎患者#
60
#Rheumatology#
51
#关节炎#
0
#类风湿#
46
#风湿关节炎#
49