JAMA Surgery:前哨淋巴结活检与淋巴结切除术对中、高等级子宫内膜癌分期的评估
2020-11-15 MedSci原创 MedSci原创
SLNB似乎是手术分期低、高EC的可行选择。
前哨淋巴结活检(SLNB)与淋巴结切除术在中、高级子宫内膜癌诊断中的准确性如何?近日,JAMA Surgery上发表了一项名为Assessment of Sentinel Lymph Node Biopsy vs Lymphadenectomy for Intermediate- and High-Grade Endometrial Cancer Staging的新研究,在这项涉及156例子宫内膜癌患者(126例组织学亚型高级别)的队列研究中,SLNB对淋巴结转移检测的敏感性为96%,阴性预测值为99%。而总共26%的淋巴结阳性肿瘤患者在淋巴结切除术边界外或需要免疫组化诊断。结果显示,SLNB对极有淋巴结转移风险的高级别子宫内膜癌患者的诊断准确性和预后能力与淋巴结切除术相似。
在这项前瞻性、多中心队列研究中(前哨淋巴结活检与淋巴结切除术中、高级子宫内膜癌分期[SENTOR]研究),纳入的患者发病时间为2015年7月1日至2019年6月30日,包括临床I期2级子宫内膜样体或高级别子宫内膜癌(EC)患者,所有患者均行SLNB后行淋巴结切除术作为参考标准。2级子宫内膜样EC患者行盆腔淋巴结清扫术(PLND),高级别子宫内膜样EC患者行PLND加腹主动脉旁淋巴结清扫术(PALND)。主要评价指标为SLNB算法的敏感性。次要结果是诊断准确性、前哨淋巴结检出率和不良事件的附加测量。
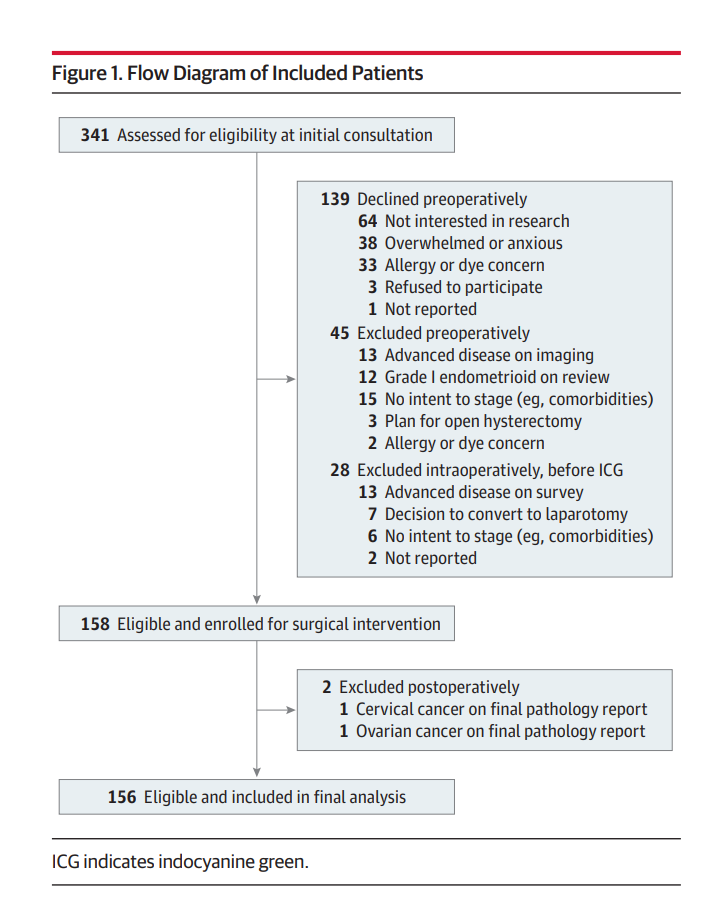
纳入患者流程图
该研究纳入了156名患者(中位年龄65.5岁),包括126种高级别EC。所有患者均行SLNB和PLND, 101例(80%)高级别EC患者同时行PALND。前哨淋巴结检出率分别为97.4% (95% CI, 93.6%-99.3%)、87.5% (95% CI, 83.3%-91.0%)和77.6%(双侧)。在27例(17%)有淋巴结转移的患者中,有26例经SLNB算法正确识别,敏感性为96% (95% CI, 81%-100%),假阴性率为4% (95% CI, 0%-19%),阴性预测值为99% (95% CI, 96%-100%)。只有1例患者(0.6%)被SLNB算法误分。27例淋巴结阳性肿瘤患者中,有7例(26%)在传统PLND边界之外或需要免疫组化诊断。
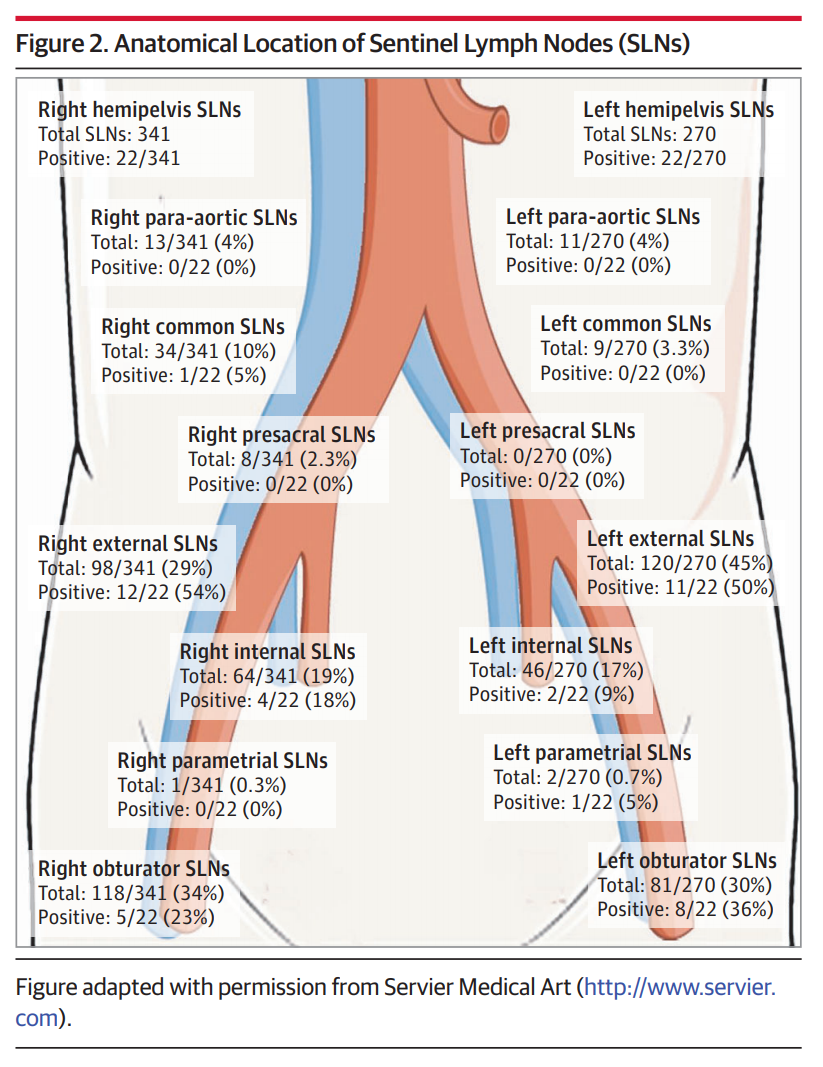
前哨淋巴结的解剖定位
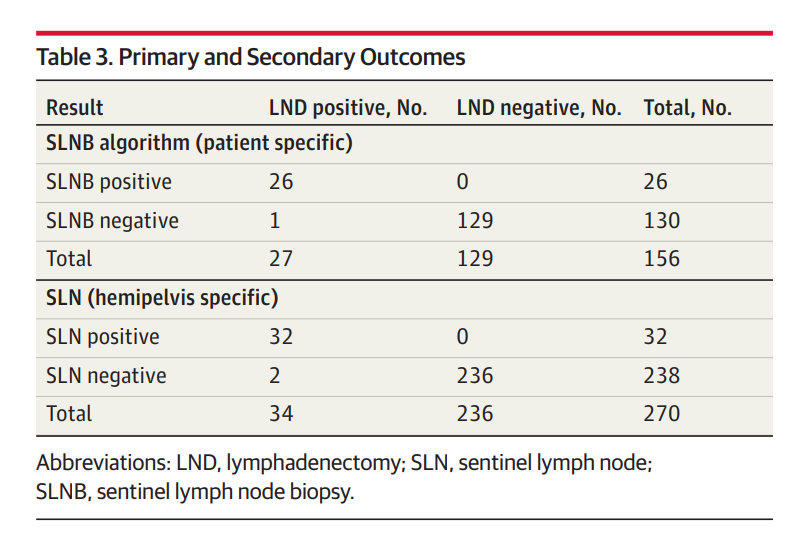
主要结果和次要结果
SENTOR研究的目的是前瞻性地评价ICG对中、重度EC患者SLNB的诊断准确性。超过96%的淋巴结阳性患者被SLNB算法正确诊断,99%的前哨淋巴结阴性患者被诊断为淋巴结阴性。这些指标与乳腺癌和黑色素瘤的观察结果相当,SLNB已成为乳腺癌和黑色素瘤的标准护理标准,并提示子宫内膜SLNB具有作为淋巴结切除术替代物试验所必需的性能特征。
SENTOR的研究还表明SLNB可以提高诊断准确性,如传统计算方法无法捕捉到的淋巴结转移的检测。14例淋巴结阳性患者(52%)仅发生前哨淋巴结转移,7例(26%)淋巴结切除术边界外或需要免疫组化诊断。这些患者不会被PLND或PALND单独识别。
总之,在本研究中,与淋巴结切除术相比,SLNB在检测高级别EC淋巴结转移疾病方面具有可接受的诊断准确性。基于本研究和现有文献,SLNB似乎是手术分期低、高EC的可行选择。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#内膜#
60
#surgery#
69
#切除术#
80
#GER#
58
#前哨淋巴结活检#
122
学习
98
棒
154
#活检#
81
#淋巴结#
61
#前哨淋巴结#
65