BMJ:呼吸困难和不寻常的胸片-案例报道
2017-03-18 xing.T MedSci原创
心包钙化认为是由于心包炎症和纤维化所导致的。该病与缩窄性心包炎相关,但不能予以诊断。将近30%的心包钙化患者有缩窄性心包炎的体征或症状。缩窄性心包炎患者中,27%-50%的患者发生心包钙化。
患者为一名70岁的男性,因呼吸短促几个月而就诊。他的胸片显示什么(如图1所示),这种情况最常见的原因是什么?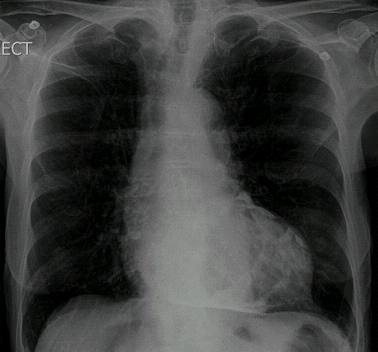
图1 胸片
回答
胸片显示心包钙化。鉴于他的症状,考虑进行超声心动图检查,由于心包钙化与缩窄性心包炎有关。尽管该病的原因通常是特发性的,缩窄性心包炎公认的原因包括感染、既往放疗或手术、胶原血管疾病。
讨论
心包钙化认为是由于心包炎症和纤维化所导致的。该病与缩窄性心包炎相关,但不能予以诊断。将近30%的心包钙化患者有缩窄性心包炎的体征或症状。缩窄性心包炎患者中,27%-50%的患者发生心包钙化。
尽管这通常是特发性的,缩窄性心包炎公认的病因包括感染、胶原血管疾病、尿毒症,以及之前的放疗、外伤性心包积血、心脏手术。从历史上看,结核感染也是心包钙化的重要原因。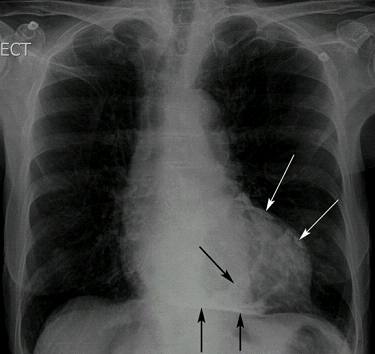
图2 胸片,黑白箭头显示左、右心室外的心包钙化
平片可区别心包钙化与心肌钙化。心包钙化常发生在右心室。当广泛的心包钙化可以延伸到左心腔,正如这个病人(图2所示)。相反,心肌钙化往往是更深层次的,常发生在心尖或左心室后壁,并可能与动脉瘤隆起相关。
学习点
对于心包钙化患者,临床医师应考虑缩窄性心包炎的可能性。
原始出处:
James SB Kho. et al. Dyspnoea and an unusual chest radiograph. BMJ2017;356:j986 doi: 10.1136/bmj.j986
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#BMJ#
0
学习了
109
#呼吸困难#
75
#胸片#
66
学习了
104
学习中,谢谢
0
学习了
0
心包钙化临床医师应该考虑缩窄性心包炎的可能
91
谢谢分享!
51
对于心包钙化患者,临床医师应考虑缩窄性心包炎的可能性,事实上,影像医师基本都会提示这个。
49