DIABETOLOGIA:新型寡核苷酸药物VE-cadherin可治疗糖尿病眼并发症的视网膜病变
2019-05-06 不详 网络
糖尿病视网膜病变的一个主要特征是视网膜血屏障的破坏,并导致黄斑水肿。我们开发了一种新型寡核苷酸药物CD5-2,它能特异性地增加内皮细胞屏障完整性关键连接蛋白的表达,即血管内皮特异性cadherin (VE-cadherin)。CD5-2可以阻止促血管生成的microRNA miR-27a沉默mRNA。本研究对CD5-2在动物眼部新生血管形成和血管渗漏模型中进行了评估,以确定其对糖尿病视网膜病变的潜
糖尿病视网膜病变的一个主要特征是视网膜血屏障的破坏,并导致黄斑水肿。我们开发了一种新型寡核苷酸药物CD5-2,它能特异性地增加内皮细胞屏障完整性关键连接蛋白的表达,即血管内皮特异性cadherin (VE-cadherin)。CD5-2可以阻止促血管生成的microRNA miR-27a沉默mRNA。本研究对CD5-2在动物眼部新生血管形成和血管渗漏模型中进行了评估,以确定其对糖尿病视网膜病变的潜在疗效。
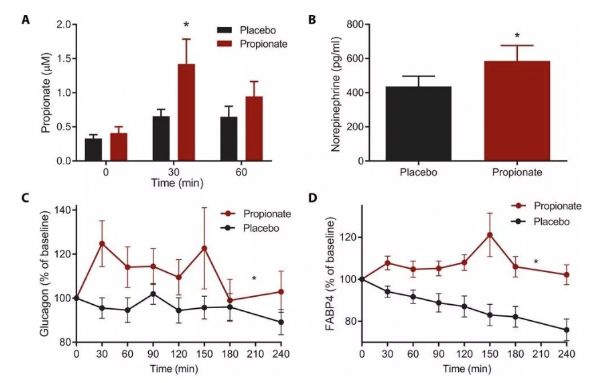
CD5-2在三种视网膜功能障碍小鼠模型中进行了测试,即条件穆勒细胞衰竭、链脲佐菌素诱导的糖尿病和氧诱导的视网膜病变。荧光素血管造影评价Muller细胞敲除模型的血管通透性。采用Evans蓝漏法测定链脲佐菌素和氧诱导视网膜病变模型的血管通透性。通过对链脲佐菌素- b4、VE-cadherin和神经胶质抗原2 (NG2)染色,观察CD5-2对链脲佐菌素-和氧诱导视网膜病变模型视网膜新生血管形成、内皮细胞间连接和周细胞覆盖率的影响。采用荧光原位杂交法测定病变视网膜中Blockmir CD5-2的定位。CD5-2 VE-cadherin表达式和糖尿病的影响retinopathy-associated途径。
结果表明,在氧诱导视网膜病变模型中,CD5-2穿透了眼睛的血管系统。在链脲佐菌素诱导的糖尿病模型和氧诱导的视网膜病变模型中,用CD5-2治疗患病小鼠可减少所有三种动物模型的血管渗漏,增强眼微血管中VE-cadherin的表达,并改善视网膜血管周细胞的覆盖率。此外,在链脲佐菌素诱导的糖尿病模型中,CD5-2降低了视网膜小胶质细胞的活化。体内CD5-2的阳性作用在体外通过增加VE-cadherin蛋白表达、SMAD2/3活性和血小板衍生生长因子B (PDGF-B)的表达进一步证实。
CD5-2具有治疗视网膜血管渗漏相关疾病的潜力,这是基于其在动物模型中易于传递和逆转三种视网膜病变的血管功能障碍和炎症方面的能力而评价的结果。
原始出处:
Ka Ka
Ting, Yang Zhao,
Therapeutic
regulation of VE-cadherin with a novel oligonucleotide drug for diabetic eye
complications using retinopathy mouse models
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#核苷酸#
75
#并发#
69
#BET#
65
#寡核苷酸#
89
#DIA#
52
#视网膜#
67
#视网膜病变#
82
谢谢MedSci提供最新的资讯
76