Cell:抑制细胞抗氧化水平,能杀死胰腺癌细胞
2016-07-29 MedSci MedSci原创
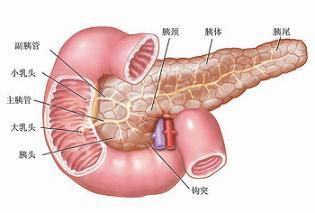
发表在7月28日《细胞》(Cell)杂志上的一项新研究揭示,降低胰腺癌细胞中抗氧化的水平可以帮助杀死它们,表明了针对这一致命癌症一种全新的治疗策略。由于胰腺位置隐蔽,早期胰腺癌很难被发现,多数患者在确诊时已是晚期,5年生存率一般不到5%。这种生长快速而且转移率高的癌症,也被称为“癌症之王”。 提高机体的抗氧化剂水平往往会抑制癌症,这已成为了流行文化中人们的普遍认知。然而,冷泉港实验室的一个研
发表在7月28日《细胞》(Cell)杂志上的一项新研究揭示,降低胰腺癌细胞中抗氧化的水平可以帮助杀死它们,表明了针对这一致命癌症一种全新的治疗策略。由于胰腺位置隐蔽,早期胰腺癌很难被发现,多数患者在确诊时已是晚期,5年生存率一般不到5%。这种生长快速而且转移率高的癌症,也被称为“癌症之王”。
提高机体的抗氧化剂水平往往会抑制癌症,这已成为了流行文化中人们的普遍认知。然而,冷泉港实验室的一个研究小组在一系列复杂的实验中证实,在胰腺细胞踏上通往癌症的道路,或已经处于恶性状态这些特殊的情况下,最不愿干的事情就是提高抗氧化剂的水平。
领导这一研究的是冷泉港实验室的David Tuveson教授。Tuveson实验室的主要研究方向是探究胰腺癌的基础生物学及发现新的诊断和治疗策略,近年取得不少重要的研究成果。
在发表于2013年PNAS杂志上的一篇研究论文中,Tuveson教授领导的一个科学家小组指出,人们一直认为,药物无法很好地穿透胰腺肿瘤是导致治疗失败的主要原因。而他们证实,还有其他的因素在起作用(PNAS:英国开发新药获突破 六天可治愈胰腺癌)。
2014年7月,在发表于《新英格兰医学》(NEJM)杂志上的一篇简短论文中,Tuveson博士和西北大学Feinberg医学院的Navdeep S. Chandel博士,提出了为何抗氧化剂不能发挥作用抑制癌症形成,以及它们实际上可能弊大于利的原因(NEJM:抗氧化剂如何加速癌症发生)(Science:抗氧化剂可能会通过作用于癌症基因的方式诱发癌症)。
2015年,在Tuveson及Hubrecht研究所所长及教授、荷兰皇家艺术与科学院院长Hans Clevers的共同领导下,研究研究开发出了一种方法不仅可以培养来自实验室小鼠模型的胰腺组织,还可培养来自人类患者的胰腺组织,由此提供了一条未来通向个体化疗法的路径。这项研究发布在在Cell杂志上(Cell:饿死癌细胞?恐怕没那么简单)。
在每个细胞中都生成了一些氧化剂和抗氧化剂,当细胞健康时它们维持在一个非常精确的平衡状态。增殖癌细胞呈现一种特殊情况:恶性细胞中生成的氧化剂越多,生成的抗氧化剂也越多,抵制了氧化增加造成的影响。没有同量的更多的抗氧化剂,恶性细胞会由于过度氧化而死亡。Tuveson领导这一冷泉港实验室研究小组从这一观点出发着手展开了研究。
Tuveson实验室的博士后研究人员Iok In Christine Chio说:“当然,这正是我们希望癌细胞所做的——让它们自身筋疲力尽。我们实验室正在测试的治疗原则就是,通过提高氧化剂在癌细胞中的水平,看是否能够导致癌前病变和恶性细胞死亡。”
大多数现有的癌症疗法,包括电离辐射治疗和化疗都依赖于氧化的杀伤能力。抗氧化剂确实对细胞健康起作用;但涉及到杀死癌细胞时,它们则是非常令人厌恶的东西。
当细胞检测到过度氧化时,它们会遵循一个叫做凋亡的内置程序完成自杀。在癌细胞中提高氧化的一种方法就是降低这些细胞中的抗氧化剂水平。Tuveson研究小组解决了如何最好地做到这一点,且不伤害健康细胞这一问题。他们将焦点放在了一个叫做NRF2的蛋白上。科学家们称它为氧化还原平衡的主要调控因子——它是人们可以调整来破坏癌细胞中氧化与还原之间精妙平衡的一个开关。
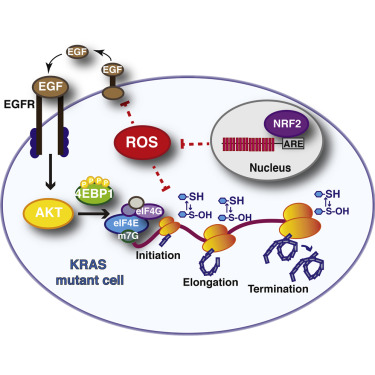
当NRF2活化时,细胞会合成谷胱甘肽(glutathione),它是一种重要的抗氧化剂。试图减少NRF2活性或是让它完全失去作用是有意义的。然而出于两个原因不可能做到这一点。第一是因为NRF2是一个转录因子。转录因子出了名难以用药物靶向。Chio说“但无论如何你大概不会想让它丧失功能。因为除了促进生成谷胱甘肽,NRF2还调控了数百个不同的基因。”你无法在不影响许多其他过程的情况下从细胞中删除它。
Tuveson、Chio和研究小组的其他成员在对实验室中培养的胰腺细胞完成了一些实验后提出了一种不同的策略,并在胰腺癌动物模型中测试了一些新的治疗方法。
利用一组胰腺类器官——从胰腺癌患者和健康胰腺处取得的胰腺细胞的球形团块,他们观察了当完全除掉NRF2时发生的事情。他们对正常、癌变前和恶性的胰腺类器官进行了测试。癌变前类器官携带着一些kras基因突变,kras基因在几乎所有的人类胰腺癌中异常。恶性类器官携带着这一kras基因突变和使得强大的肿瘤抑制基因p53失活的一种突变。在大多数恶性肿瘤中都可以看到这种突变与kras突变一起。
这些实验提供了一个至关重要的线索:研究小组看到当缺失NRF2时, 细胞中将来自基因的信息翻译为蛋白质的机器对氧化剂和抗氧化剂之间平衡的波动非常敏感。重要地是,在正常胰腺细胞中蛋白质合成不受影响。Chio说:“当我们看到这一现象时我们非常兴奋,这意味着我们可以寻找一种方法来减少抗氧化剂,蛋白质合成将只在癌前和恶性细胞中受影响,这是一种潜在强大的治疗策略。”
这种现象叫做合成致死性。它发生在影响健康和不健康细胞的一种情况只对不健康细胞致命之时。
研究小组提出了一种二药鸡尾酒,他们将鸡尾酒传送到胰腺癌模型小鼠体内。其中一种药物AKT抑制剂旨在抑制促成蛋白质合成的翻译起始。另一种药物BSO抑制了谷胱甘肽合成。
单给予AKT抑制剂只在小鼠模型和人类患者中产生了轻微的生存利益。Chio说:“我们希望通过联合它们与BSO,我们能够生成协同作用,提高它的疗效。”事实上,这一策略模拟了当他们在癌细胞中敲除NRF2或降低其水平时生物化学上发生的事件。这是让BSO搭乘AKT抑制剂便车的理论基础。
Chio 说:“这是我们的胰腺类器官如此有价值的地方。我们可以验证这一想法,看看这种方法是否合成致死——它确实提高了AKT抑制剂的杀伤能力,而这种协同作用不存在于正常胰腺细胞中。”换句话说,正常胰腺细胞不会受到这种治疗的损伤。
研究小组在新论文中报告了胰腺癌小鼠模型中的协同效应,证实了通过降低癌细胞抗氧化剂水平来杀死更多癌症这一概念。对于小鼠中记录的生存利益不完全满意,他们认为可通过组合不同的翻译抑制剂和抗氧化剂合成抑制剂来优化这一疗法。这项工作正在进行中。
这种方法有可能与kras突变让细胞踏上恶变道路的其他癌症有关。这包括某些类型的肺癌和乳腺癌。
Tuveson说:“胰腺癌利用了NRF2作为它的亲信促进坏行为,但以往并不清楚其细节。通过开发类器官模型,冷泉港实验室蛋白质组学专家Christine探究了NRF2的基础生物学,以揭示这一蛋白的分子基础,由此提出了一些针对患者的新疗法。我们希望在不久的未来将Christine的研究发现转化为早期临床试验。”
原始出处:
Iok In Christine Chio, Seyed Mehdi Jafarnejad, Mariano Ponz-Sarvise10, Youngkyu Park, Keith Rivera, Wilhelm Palm, John Wilson, Vineet Sangar, Yuan Hao, Daniel Öhlund, Kevin Wright, Dea Filippini, Eun Jung Lee, Brandon Da Silva, Christina Schoepfer, John Erby Wilkinson, Jonathan M. Buscaglia, Gina M. DeNicola, Herve Tiriac, Molly Hammell, Howard C. Crawford, Edward E. Schmidt, Craig B. Thompson, Darryl J. Pappin, Nahum Sonenberg, David A. TuvesoncorrespondencePress enter key for correspondence informationemail.NRF2 Promotes Tumor Maintenance by Modulating mRNA Translation in Pancreatic Cancer. Cell July 28, 2016. http://dx.doi.org/10.1016/j.cell.2016.06.056
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
72
#CEL#
68
stop
98
#癌细胞#
56
肿瘤的治疗任重道远,肿瘤到底该怎么治疗!
2
厉害的研究
84
受益匪浅。谢谢!
101
抗氧化剂剂反而促进肿瘤发展!促进细胞内氧化应激水平,有助于杀伤肿瘤细胞
94