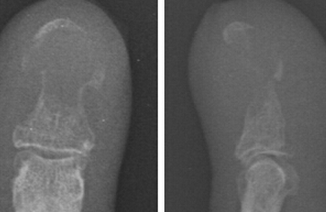
女性,61岁,因左手大拇指甲床出现畸形并伴有无痛性溃疡史3年来院就诊。据该女患者主诉,以往她的左手大拇指没有出现过创伤史或长过疣。当年就诊时会诊医生诊断其患的是甲沟炎,并予抗生素进行治疗。但治疗效果并不理想。通过体格检查发现,其左手大拇指甲床呈现出不规则溃疡病变以及色素沉着,甲床的远端出现断裂消失。切开活检,活检标本的组织病理学检查显示中度分化的鳞状细胞癌。真菌涂片检验结果显示阴性。胸片和全身锝-99骨扫描未见有癌细胞转移的迹象。最后,该女患者接受会诊医生的建议,经手术彻底切除病灶。一般情况下,甲床的鳞状细胞癌是非常罕见的,而这种疾病往往可能是由如银屑病、寻常疣、甲沟炎和甲癣等疾病发展而来。因此,对于本案例的诊断在临床上很容易被漏诊从而导致治疗延误。原始出处:Feily A.Squamous-Cell Carcinoma of the Nail Bed. N Engl J Med. 2015 Dec 10;373(24):2357.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#细胞癌#
86
#指甲#
64
少见
105
罕见
166
很少见
159