MYSTIC研究:durvalumab与tremelimumab联用无法显著提高肺癌患者的生存率
2018-11-18 MedSci MedSci原创
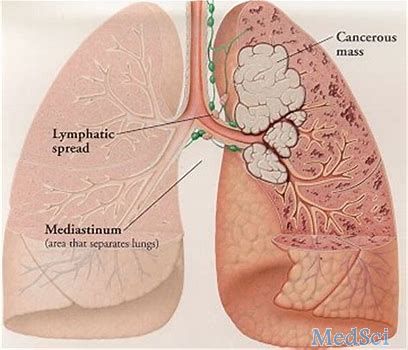
阿斯利康近日宣布,在III期MYSTIC研究中,与标准铂类化疗相比,PD-L1抑制剂Imfinzi(durvalumab)作为单药疗法及与抗CTLA4抗体tremelimumab的联合使用未能显著提高初治IV期非小细胞肺癌(NSCLC)患者的总生存期(OS)。
阿斯利康近日宣布,在III期MYSTIC研究中,与标准铂类化疗相比,PD-L1抑制剂Imfinzi(durvalumab)作为单药疗法及与抗CTLA4抗体tremelimumab的联合使用未能显著提高初治IV期非小细胞肺癌(NSCLC)患者的总生存期(OS)。阿斯利康首席医疗官Sean Bohen说:“我们对这些结果缺乏统计意义而感到失望”。早在去年,阿斯利康公布了MYSTIC研究的初步结果,Imfinzi和tremelimumab的联合未能显著改善患者的无进展生存期(PFS)。
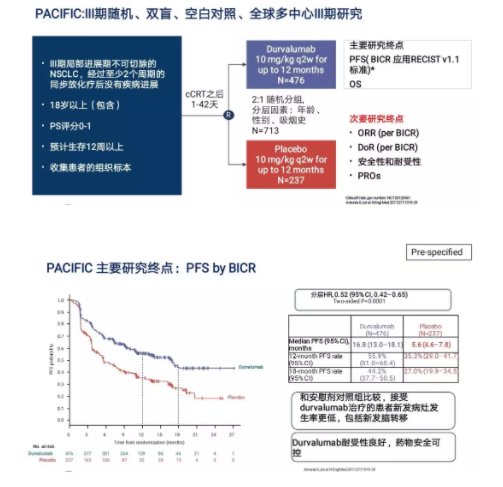
该研究将患有EGFR和ALK野生型,局部晚期或转移性IV期非小细胞肺癌(NSCLC)患者随机分组接受Imfinzi单药治疗、Imfinzi联合tremelimumab或标准铂类化疗。该试验的主要终点包括Imfinzi单药治疗、Imfinzi和tremelimumab联合使用的PFS和OS。阿斯利康表示,尽管OS结果不具有显著的统计学意义,但Imfinzi单药治疗的危险比(HR)为0.76,而联合治疗的HR为0.85。阿斯利康表示将在不同的患者亚组中进一步分析相关数据,以挖掘Imfinzi和tremelimumab联用的有效性的证据。
原始出处:
http://www.firstwordpharma.com/node/1604929#axzz5XAXlsKfr
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肺癌患者#
67
#TREM#
89
#mAb#
96
#REM#
106
#生存率#
66
#Tremelimumab#
96