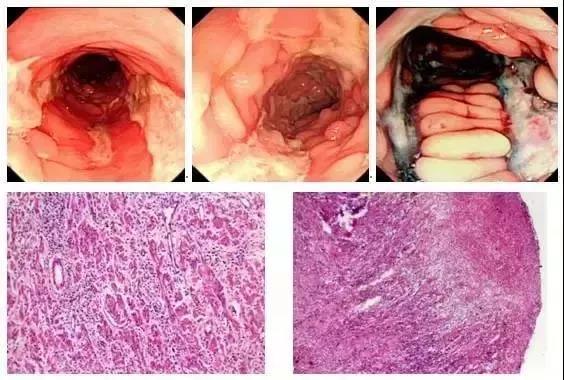
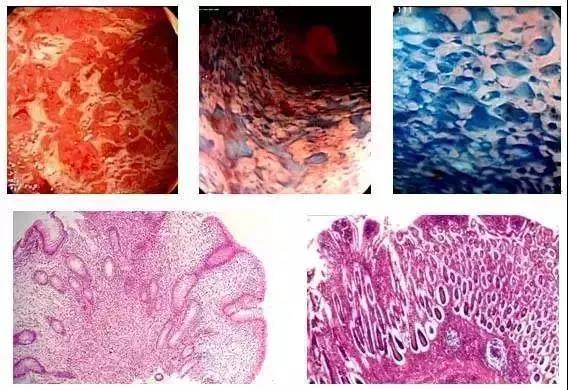
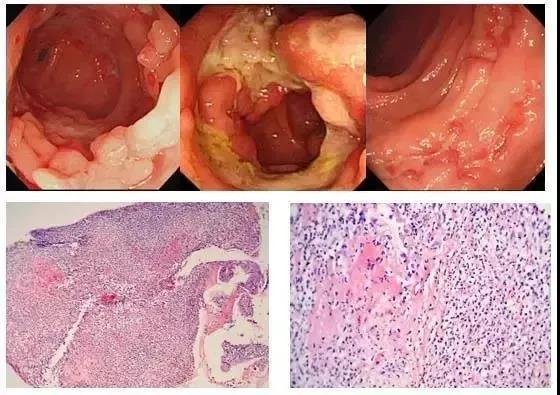
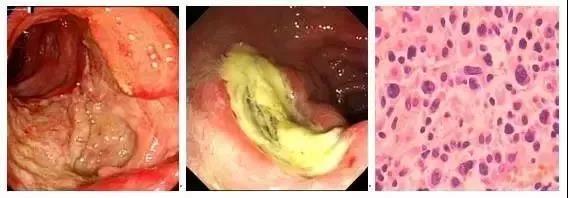
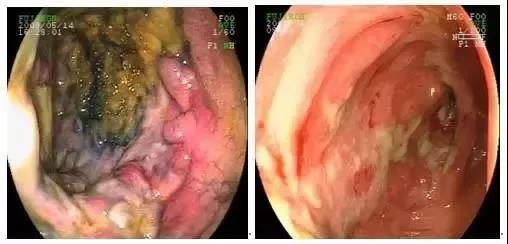
六种肠道消化溃疡性疾病的内镜鉴别诊断
2019-07-08 李明松 CCMTV消化频道
结肠镜检查中,肠道溃疡性病变常见,包括回肠末端溃疡、回盲瓣溃疡和盲肠溃疡和结肠溃疡。常见的相关疾病有感染性肠炎、克罗恩病、溃疡性结肠炎、肠结核、肠型淋巴瘤、白塞病、缺血性肠炎和肠癌等。这些疾病虽然结肠镜下均以肠道溃疡为主,但其特点各不相同。今天我们就回顾学习一下临床容易混淆的克罗恩病、溃疡性结肠炎、肠结核、肠型淋巴瘤、白塞病、缺血性肠炎的结肠镜下特点及其病理学特征。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了
106
学习了
104
好
138
#溃疡性#
73
学习了,谢谢分享。
137
#内镜#
72
#鉴别诊断#
89
好
112
学习了
140
不错
97